Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
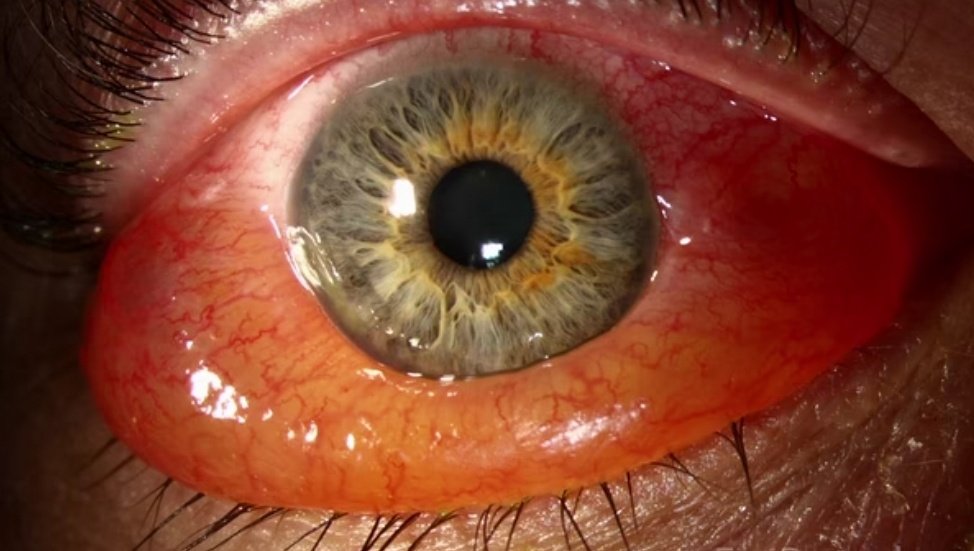
Chemosis
👁️ Chemosis (Conjunctival oedema) — Causes & Management
🧠 Chemosis = swelling/oedema of the conjunctiva (often looks like “jelly” or ballooning around the cornea). Pathophysiology is usually either ↑ vascular permeability (allergy/inflammation/infection) or venous/lymphatic congestion (orbital pressure, thyroid eye disease, impaired venous drainage). The key clinical skill is spotting the few dangerous causes where chemosis is a marker of orbital pathology rather than simple conjunctivitis.
✅ First assessment (always)
- 📌 Check vision (acuity), pupils (RAPD), and pain level.
- 👀 Look for proptosis, reduced eye movements, diplopia, corneal exposure, photophobia.
- 🌡️ Ask about fever, sinus symptoms, trauma/surgery, contact lenses, anaphylaxis symptoms.
- 🧪 If discharge: watery vs mucopurulent; consider fluorescein if pain/photophobia/contact lenses (corneal involvement).
🚨 Red flags (same-day urgent ophthalmology / ED)
- 🔻 Reduced visual acuity or RAPD
- 😖 Severe pain, marked photophobia, or headache
- 👁️🗨️ Proptosis, restricted eye movements, diplopia
- 🌡️ Fever/toxicity, sinusitis + eye signs (think orbital cellulitis)
- 🩸 Recent facial/orbital trauma or eye surgery (think retrobulbar haemorrhage)
- 🧪 Chemical splash / alkali injury
- 🦠 Copious purulent discharge + rapid swelling (think gonococcal infection)
🧩 Causes of chemosis
- 🌼 Allergic conjunctivitis (itching, watery discharge, lid swelling; often bilateral)
- 🦠 Viral conjunctivitis (gritty, watery, contagious; pre-auricular nodes)
- 🧫 Bacterial conjunctivitis (mucopurulent discharge, lids stuck; usually mild)
- 🦠 Chlamydial conjunctivitis (chronic redness/discharge; follicular changes)
- ☣️ Severe hyperacute conjunctivitis (e.g., gonococcal) — can cause dramatic chemosis
- 🧠 Orbital cellulitis / post-septal infection (chemosis + proptosis + painful/restricted EOM)
- 🩸 Trauma / post-op swelling; retrobulbar haemorrhage (time-critical vision threat)
- 🦋 Thyroid eye disease (exposure, lid retraction, proptosis; chemosis from congestion)
- 🧠 Venous outflow obstruction (e.g., cavernous sinus thrombosis, carotid–cavernous fistula, SVC obstruction)
- 😮💨 Angioedema/anaphylaxis (rapid onset lid/conjunctival swelling + systemic features)
- 🌙 Exposure/lagophthalmos (dryness + conjunctival oedema, especially overnight)
💊 Management (practical approach)
1) If red flags → urgent escalation
- 📞 Same-day ophthalmology/ED if any red flags (vision threat/orbital disease).
- 🧠 Suspected orbital cellulitis/CST: treat as emergency (IV antibiotics + imaging per local pathway).
- 🩸 Suspected retrobulbar haemorrhage: emergency decompression pathway (do not delay).
- 🧪 Chemical injury: immediate irrigation + urgent ophthalmology.
2) If uncomplicated (no red flags) → treat the common causes
🌼 Allergic chemosis
- 🧊 Cold compresses; avoid rubbing (rubbing worsens mast-cell mediator release).
- 💧 Lubricants (preservative-free artificial tears) regularly.
- 🧪 Topical antihistamine/mast-cell stabiliser drops (e.g., olopatadine/cromoglicate depending on local formulary).
- 💊 Oral non-sedating antihistamine if systemic allergy symptoms.
- 🧑⚕️ If severe/persistent: consider short supervised course topical steroid only with ophthalmology input (risk of HSV/glaucoma).
🦠 Viral conjunctivitis
- 💧 Lubricants + cold compresses; hygiene advice (handwashing, avoid sharing towels).
- 🚫 Avoid routine antibiotics (usually self-limiting).
- 🚩 If significant photophobia/pain or reduced vision: consider keratitis → urgent eye review.
🧫 Mild bacterial conjunctivitis
- 🧼 Lid hygiene, warm compress if crusting.
- 💊 Consider topical antibiotic if marked purulence, contact-lens wearer, or not improving (local formulary e.g., chloramphenicol).
- 🧴 Stop contact lenses until fully resolved; replace lenses/case to prevent reinfection.
🦠 Chlamydial / hyperacute (gonococcal) suspicion
- 📞 Same-day sexual health/ophthalmology advice.
- 💉 Gonococcal eye infection is an emergency (systemic therapy + urgent ophthalmology; corneal perforation risk).
🦋 Thyroid eye disease / exposure-related chemosis
- 💧 Aggressive lubrication (drops by day, ointment at night), consider taping lids closed overnight if exposure.
- 🚭 Smoking cessation (major modifiable risk factor for TED severity).
- 🧑⚕️ Refer to ophthalmology/TED service if proptosis, diplopia, pain, or corneal exposure.
🏠 Patient advice
- ✅ Seek urgent help if vision worsens, pain increases, new diplopia, or swelling rapidly progresses.
- 🧼 Avoid rubbing; wash hands; don’t share towels/makeup.
- 👓 Avoid contact lenses until symptoms fully settle.
🔑 Clinical pearl: chemosis is a sign, not a diagnosis. The “big divider” is whether there are features of orbital disease or vision compromise. If the eye is painful, proptosed, movement-limited, febrile, or vision is reduced, treat it as urgent until proven otherwise.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology