| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
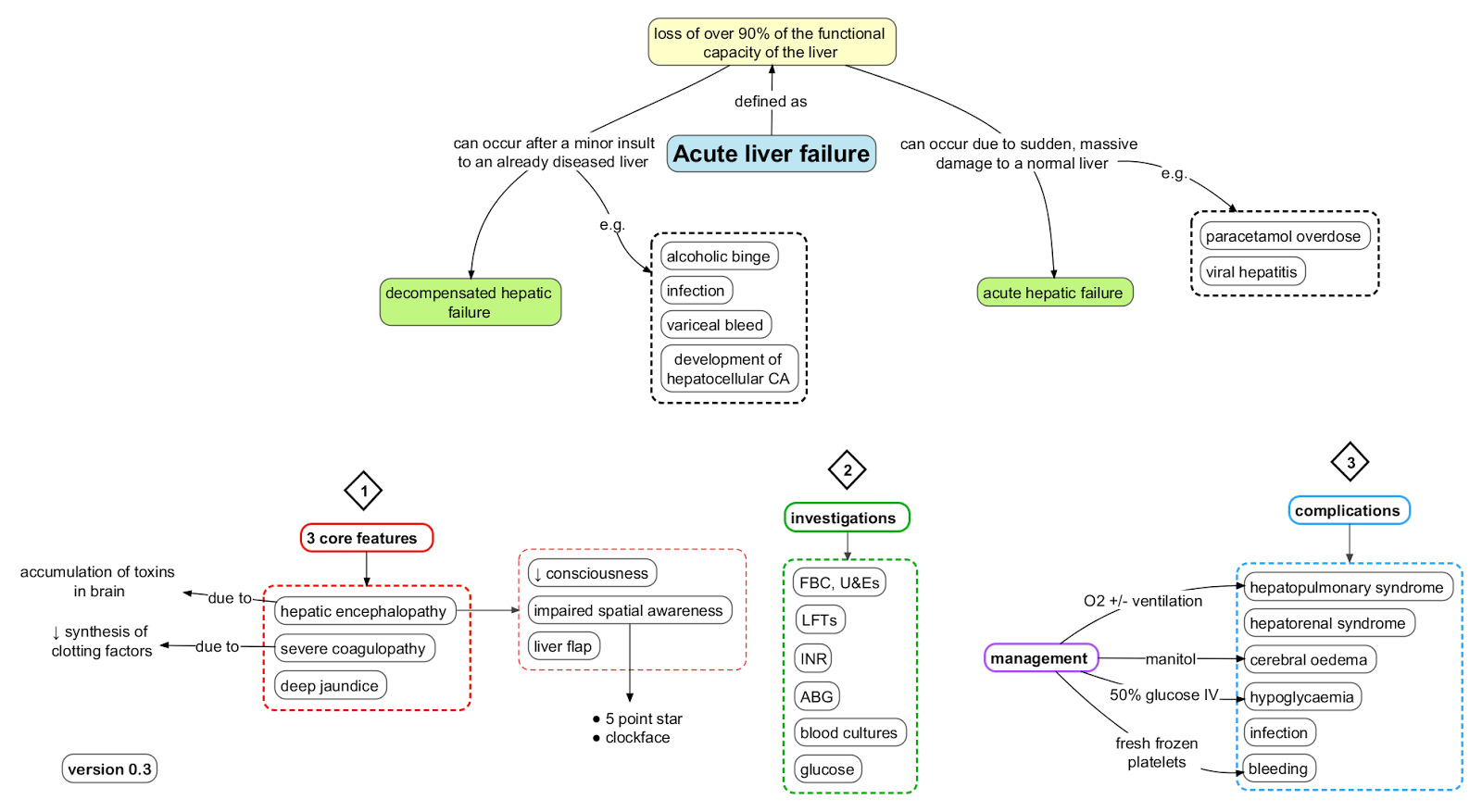
Acute Liver Failure
Related Subjects: |Chronic liver disease |Liver Function Tests |Ascites Assessment and Management |Budd-Chiari syndrome |Alcoholism and Alcoholic Liver Disease |Liver Transplantation
⚠️ Acute Liver Failure (ALF) is acute primary liver dysfunction in a patient without pre-existing chronic liver disease. In hyperacute cases, jaundice-to-encephalopathy develops within <1 week (often due to paracetamol toxicity or viral hepatitis A, B, E). Red flags: coagulopathy, high transaminases, ↑ bilirubin, and altered consciousness → may progress to coma & death.
Classification: Jaundice → Encephalopathy Interval
| Classification | Time Gap | Common Causes | Key Features |
|---|---|---|---|
| Hyperacute | < 1 week | 💊 Paracetamol, viral hepatitis | High risk cerebral oedema |
| Acute | 1 week – 1 month | Drugs, viruses, autoimmune | Cerebral oedema possible |
| Subacute | 1 – 3 months | Drugs, viruses, unknown | Less cerebral oedema |
ℹ️ About
- 📊 Incidence: ~10 cases/million/year (developed countries).
- 👩 Typically affects young, previously healthy adults.
- Fulminant hepatic failure: encephalopathy within 8 weeks of symptoms, no prior liver disease.
- 🔎 Diagnostic criteria: Injury <26 weeks, INR >1.5, altered mental status, no cirrhosis.
Key Findings
- 🟡 Jaundice, elevated bilirubin.
- 📈 ALT/AST very high.
- 🩸 Coagulopathy (↑ PT/INR).
- 🧠 Encephalopathy: confusion → coma.
Causes of ALF
- 🦠 Viral (40–70%): HAV, HBV, HCV, HDV, HEV, EBV, CMV, HSV.
- 💊 Drugs/Toxins (20%): Paracetamol (UK’s most common), isoniazid, phenytoin, halothane, ecstasy.
- 🛡️ Autoimmune hepatitis.
- 🔬 Metabolic: Wilson’s disease, acute fatty liver of pregnancy.
- 🩺 Vascular: Budd–Chiari syndrome.
- 🤰 Pregnancy-related: HELLP syndrome.
- 🐀 Others: Leptospirosis, yellow fever, Reye’s syndrome (aspirin in children).
- ❓ 20–30% remain idiopathic.
🩺 Clinical Features
- 📖 History: Drug exposure, toxins, infection.
- 🤢 Symptoms: Jaundice, nausea, bleeding, hypoglycaemia.
- 🧠 Encephalopathy signs: Asterixis, fetor hepaticus, apraxia.
- Stigmata of chronic disease usually absent.
- Grades of encephalopathy: 1 = disoriented → 4 = coma.
🔎 Investigations
- 🧪 Bloods: FBC, U&E, LFT, clotting, ABG (metabolic acidosis), ammonia, viral serology, autoimmune screen, Wilson’s tests, pregnancy test, HIV.
- 🖥️ Imaging: Liver USS + Doppler (exclude Budd–Chiari).
- 🧫 Consider biopsy if unclear cause & coagulopathy corrected.
General Management
- 🛌 Admit to high-dependency/ICU; involve hepatology early.
- 🔄 ABC support: oxygen, IV fluids, airway if encephalopathy ≥3.
- 🍬 IV dextrose infusion for hypoglycaemia.
- 🩸 Coagulopathy: Vitamin K, FFP/platelets if bleeding or invasive procedures.
- 💩 Lactulose for encephalopathy (2–3 soft stools/day).
- 🧠 Prevent ↑ ICP: head up 20°, avoid hypotension/hypoxia, mannitol if cerebral oedema.
- 🚑 Early referral to liver transplant centre if criteria met.
Cause-Specific Management
- 💊 Paracetamol overdose → IV N-acetylcysteine (NAC) immediately.
- 🛡️ Autoimmune hepatitis → steroids (e.g. prednisolone) if infection excluded.
- 🍄 Mushroom (Amanita) → IV penicillin G ± silymarin; urgent transplant eval.
- 🤰 Pregnancy: Deliver fetus (acute fatty liver, HELLP).
- 🧬 Wilson’s disease → urgent transplant.
- 🦠 Viral hepatitis → supportive ± antivirals in selected cases (HSV, HBV).
- 🩸 Budd–Chiari → anticoagulation, thrombolysis, shunt, or transplant.
⚠️ Complications
- ⚡ Hypoglycaemia.
- 🩸 Coagulopathy & bleeding.
- 🧠 Cerebral oedema → herniation risk.
- 🧬 Infections (sepsis risk high).
- ⛑️ Renal failure (Hepatorenal syndrome).
References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
