Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Glioblastoma
Related Subjects: |Brain tumours |Astrocytomas |Brain Metastases |Tuberous sclerosis |Turcot's syndrome |Lhermitte Duclos Disease |Oligodendroglioma |Acute Hydrocephalus |Intracranial Hypertension |Primary CNS Lymphoma (PCNSL) |Astrocytomas |Glioblastoma
Glioblastoma is the most aggressive primary malignant brain tumour in adults and is classified as a WHO Grade 4 astrocytic tumour. It is characterised by rapid growth, diffuse infiltration into surrounding brain tissue, and profound resistance to therapy. Despite advances in surgery, radiotherapy, and chemotherapy, prognosis remains poor, making understanding its biology and management essential for clinicians.
Epidemiology
- Most common malignant primary brain tumour in adults.
- Peak incidence in the 6th–7th decades of life.
- Slight male predominance.
- Rare in children, where molecular features differ significantly.
Pathophysiology
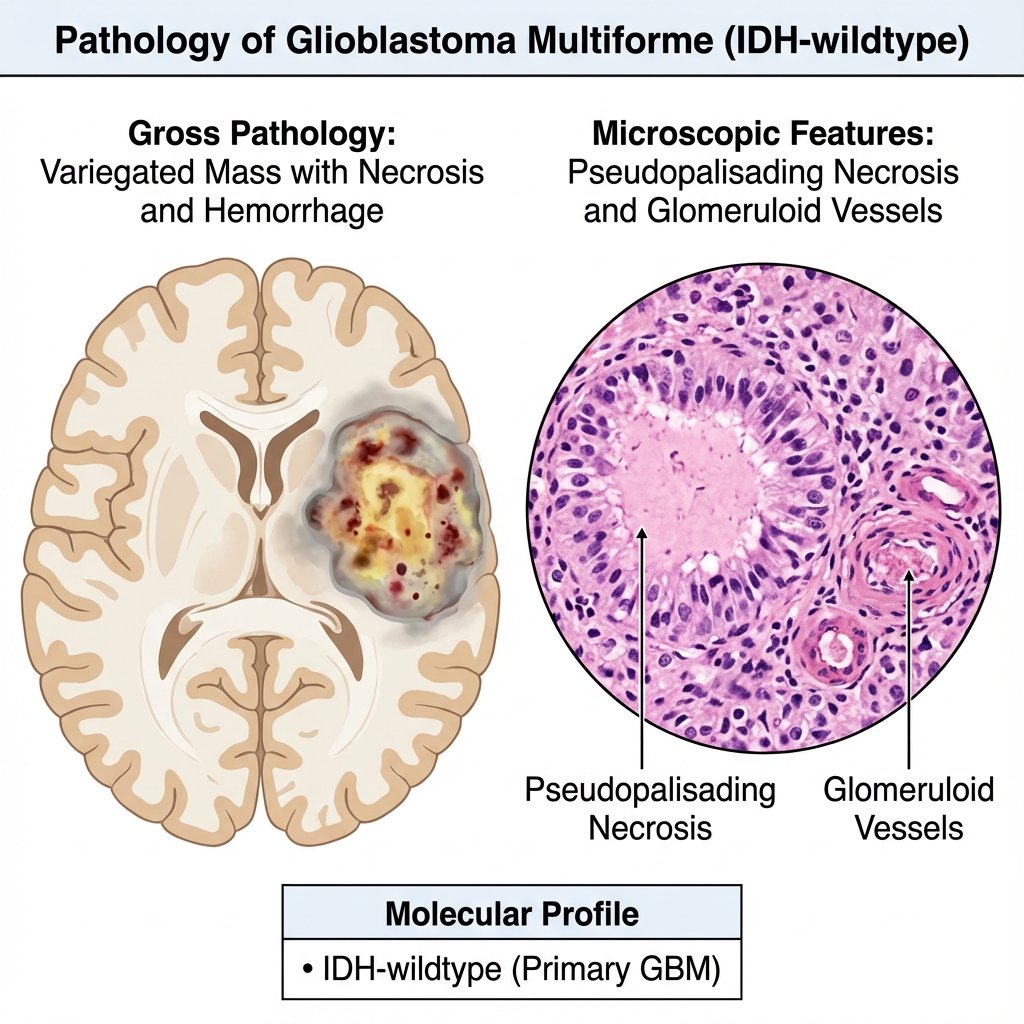
Glioblastomas arise from astrocytic lineage cells or neural stem cells that acquire multiple oncogenic mutations. Their lethality stems from diffuse infiltration along white matter tracts, making complete surgical resection impossible. Rapid angiogenesis and areas of hypoxia drive further genetic instability and aggressive behaviour.
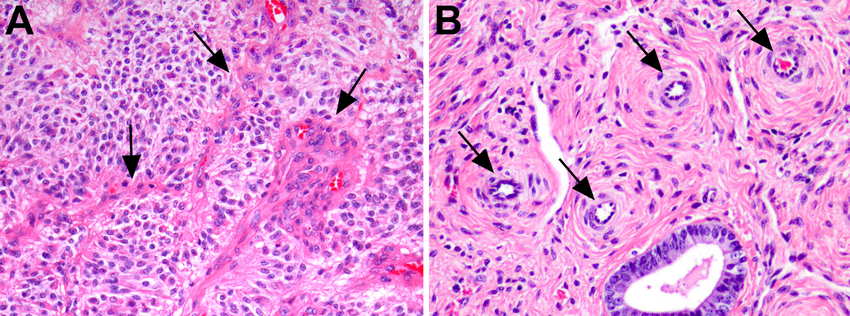
- Pseudopalisading necrosis: hallmark histological feature caused by tumour hypoxia.
- Microvascular proliferation: abnormal leaky vessels driven by VEGF.
- Infiltrative growth: tumour cells extend far beyond visible margins.
Molecular Classification (WHO 2021)
Modern classification integrates molecular genetics with histology. Adult glioblastoma is defined as an IDH-wildtype diffuse astrocytic tumour with specific molecular features, even if classical histology is incomplete. This molecular shift reflects improved prognostic accuracy and trial stratification.
- IDH-wildtype status (key defining feature).
- TERT promoter mutations.
- EGFR amplification or mutation.
- Chromosomal +7 / −10 signature.
Clinical Presentation
Symptoms depend on tumour location and mass effect. Rapid progression over weeks to months is typical, distinguishing GBM from lower-grade gliomas. Raised intracranial pressure and focal neurological deficits are common.
- Persistent or progressive headache (often morning-predominant).
- New-onset seizures in adults.
- Focal deficits such as weakness, aphasia, or visual field loss.
- Cognitive and personality changes.
Neuroimaging
MRI with contrast is the imaging modality of choice. Radiological features reflect necrosis, angiogenesis, and surrounding vasogenic oedema. Advanced imaging helps differentiate GBM from mimics such as abscess or metastasis.
- Irregular ring-enhancing mass on T1 post-contrast.
- Central necrosis with heterogeneous signal.
- Extensive surrounding T2/FLAIR oedema.
- Elevated perfusion and restricted diffusion in solid tumour regions.
Diagnosis
Definitive diagnosis requires histological confirmation, usually obtained via surgical resection or stereotactic biopsy. Tissue sampling allows both morphological assessment and molecular profiling, which is now essential for classification and management planning.
- Surgical resection where safely feasible.
- Stereotactic biopsy if lesion is deep or unresectable.
- Mandatory molecular testing.
Management
Treatment is multimodal and palliative in intent. The aim is maximal tumour control while preserving neurological function. UK practice follows neuro-oncology MDT decision-making with early palliative care involvement.
- Maximal safe surgical resection.
- Radiotherapy (typically 60 Gy in 30 fractions).
- Concurrent and adjuvant temozolomide chemotherapy.
- Corticosteroids for cerebral oedema.
Prognosis
Glioblastoma carries a poor prognosis due to its infiltrative nature and treatment resistance. Median survival is approximately 12–18 months, with long-term survival rare. Molecular features and functional status strongly influence outcomes.
- Median survival: ~12–18 months.
- Better outcomes with good performance status.
- MGMT promoter methylation predicts better response to temozolomide.
Key Learning Points
- Glioblastoma is defined by molecular criteria, not histology alone.
- Diffuse infiltration explains inevitable recurrence.
- Management is multidisciplinary and primarily palliative.
- Early honest prognostic discussions are essential in UK practice.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology