🧠 Introduction
- 🩸 Angiography visualises the lumen of blood vessels — the “pipes” of the circulation. It helps identify narrowing, occlusion, beading, dissection, aneurysm, or vascular spasm in stroke and other cerebrovascular diseases.
- 🧬 It can detect vascular malformations and track contrast movement temporally (through arterial, capillary, and venous phases) and spatially (in 3D reconstruction).
- 🧲 Modalities include X-ray–based (DSA/CTA) and MRI–based (MRA) techniques.
The gold standard remains digital subtraction angiography (DSA), although CTA and MRA have greatly reduced the number of diagnostic catheter angiograms.
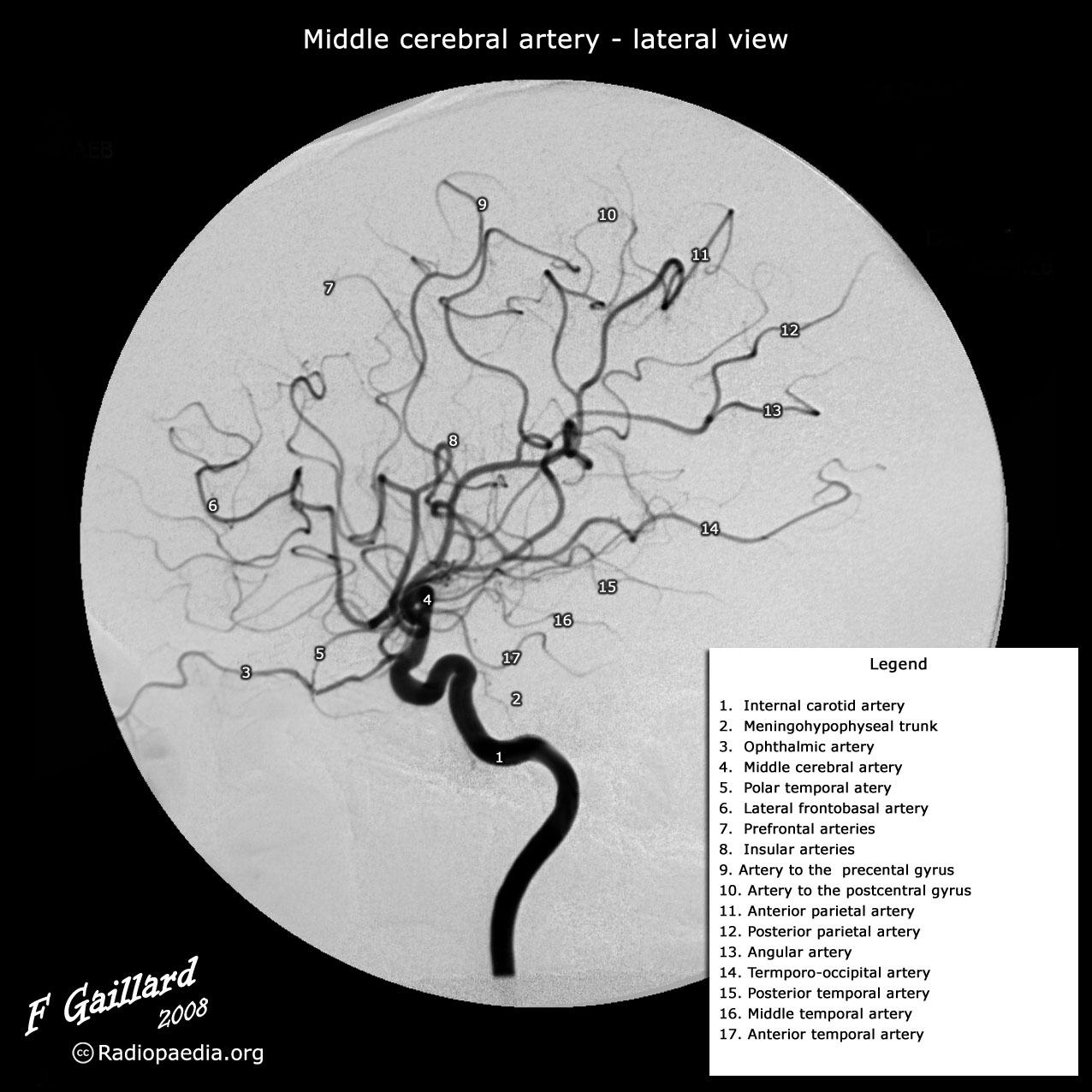
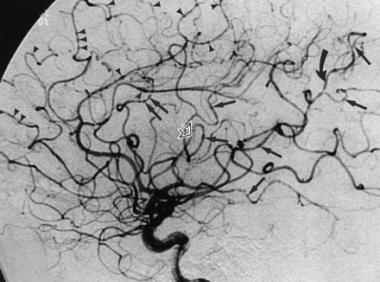
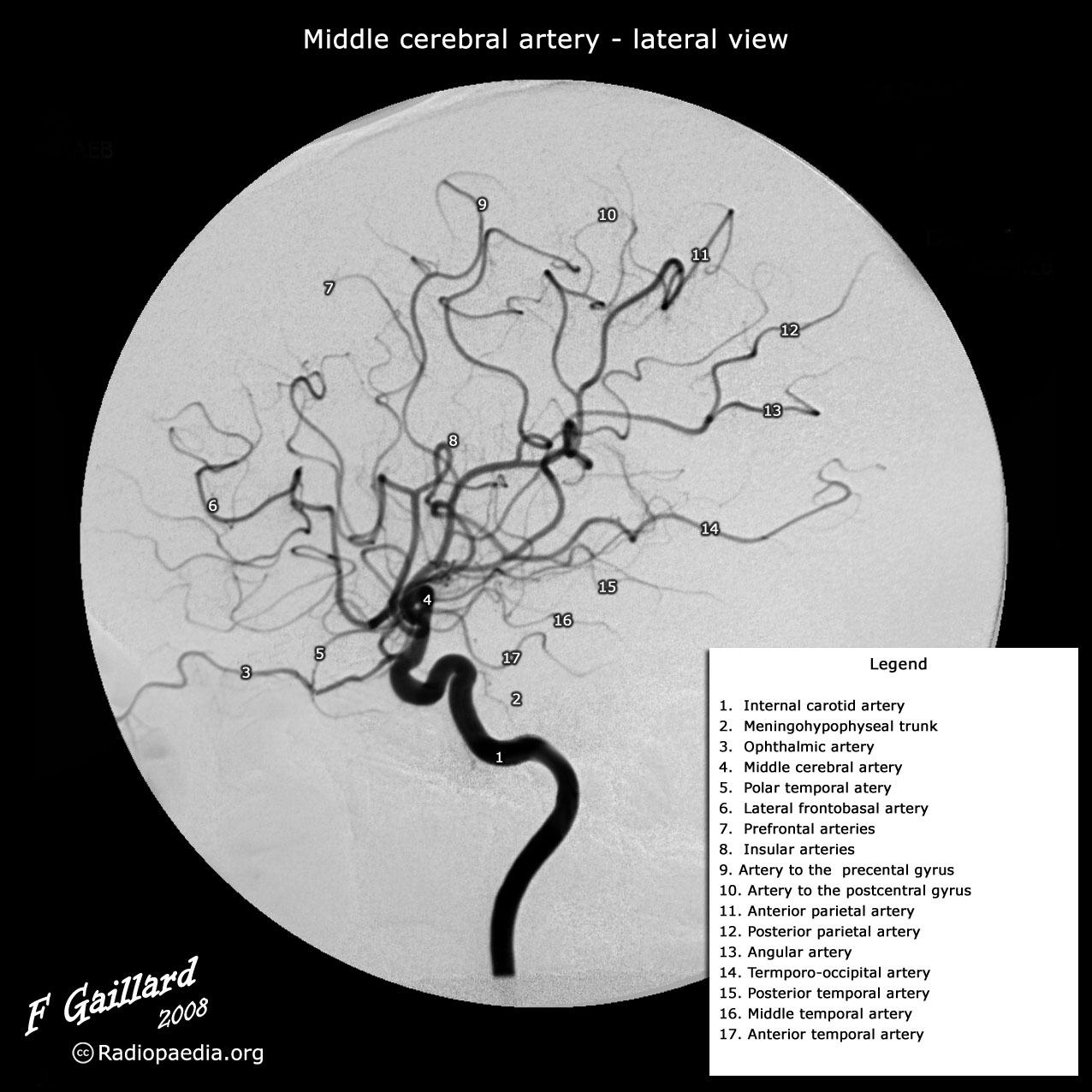
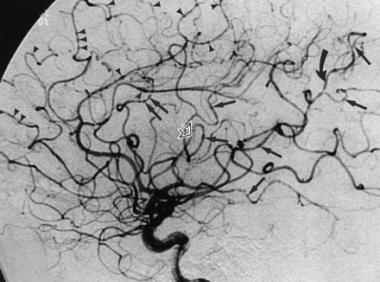
🎥 Cerebral Digital Subtraction Angiography (DSA)
- 🏅 Gold standard for vessel imaging — provides the highest spatial and temporal resolution.
- ⚙️ Technique: Catheter introduced (usually via femoral artery; radial increasingly common) → contrast injected (≈5 mL per artery) → dynamic X-ray sequence. Computer subtraction removes bone for a clear vascular image.
- 🕒 Procedure time: 20–30 min under local anaesthetic.
Risks: ≈1% stroke, 0.1% mortality, vascular injury, or contrast reaction.
- 📈 Indications: used when findings will alter management — e.g. aneurysm, AVM, vasculitis, pre-operative embolisation.
CTA can sometimes outperform DSA for aneurysm detection.
| 📋 Indications for DSA |
|---|
- Subarachnoid haemorrhage (detect aneurysm or AVM)
- Suspected carotid or vertebral dissection (if MRI inconclusive)
- Intracerebral haemorrhage with suspected AVM (young, lobar, normotensive)
- Extracranial/intracranial atheroma evaluation
- Venous sinus thrombosis (if MRI equivocal)
- Highly vascular CNS tumour (for pre-operative embolisation)
|
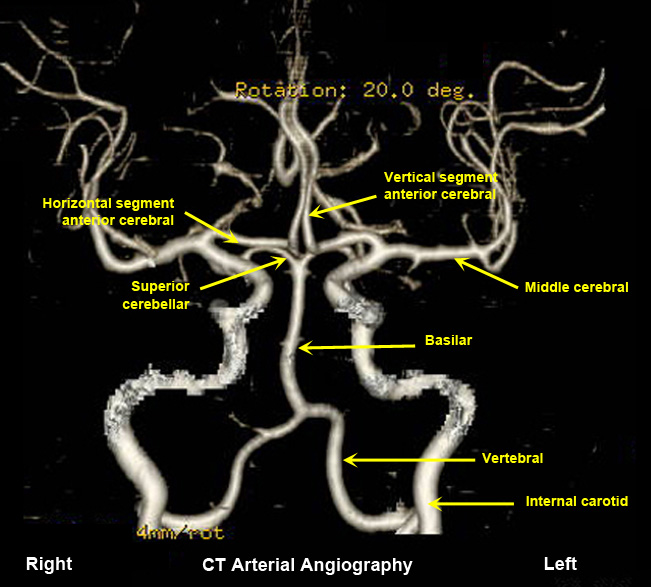
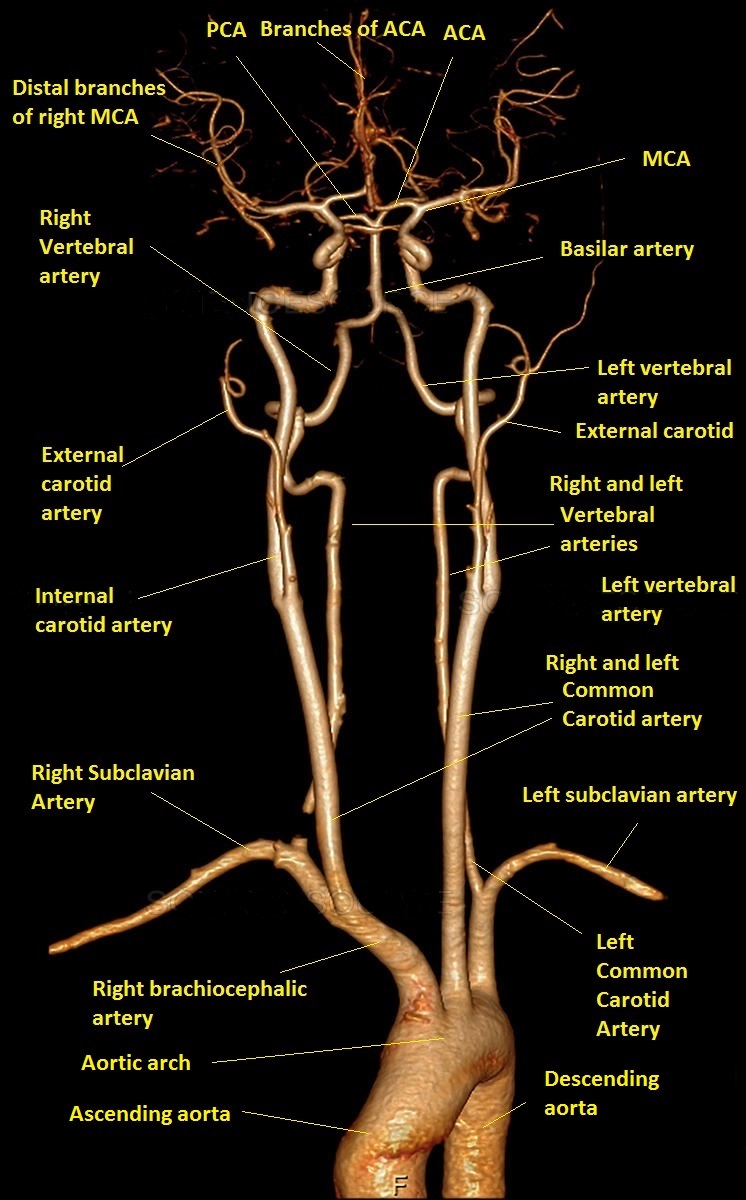
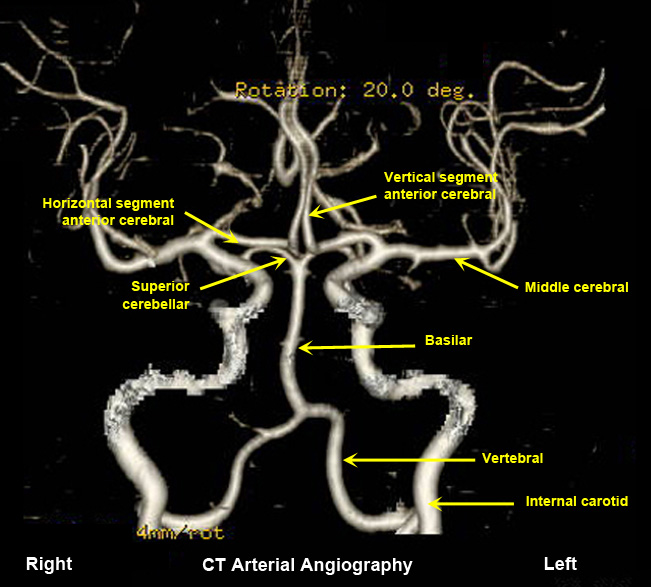
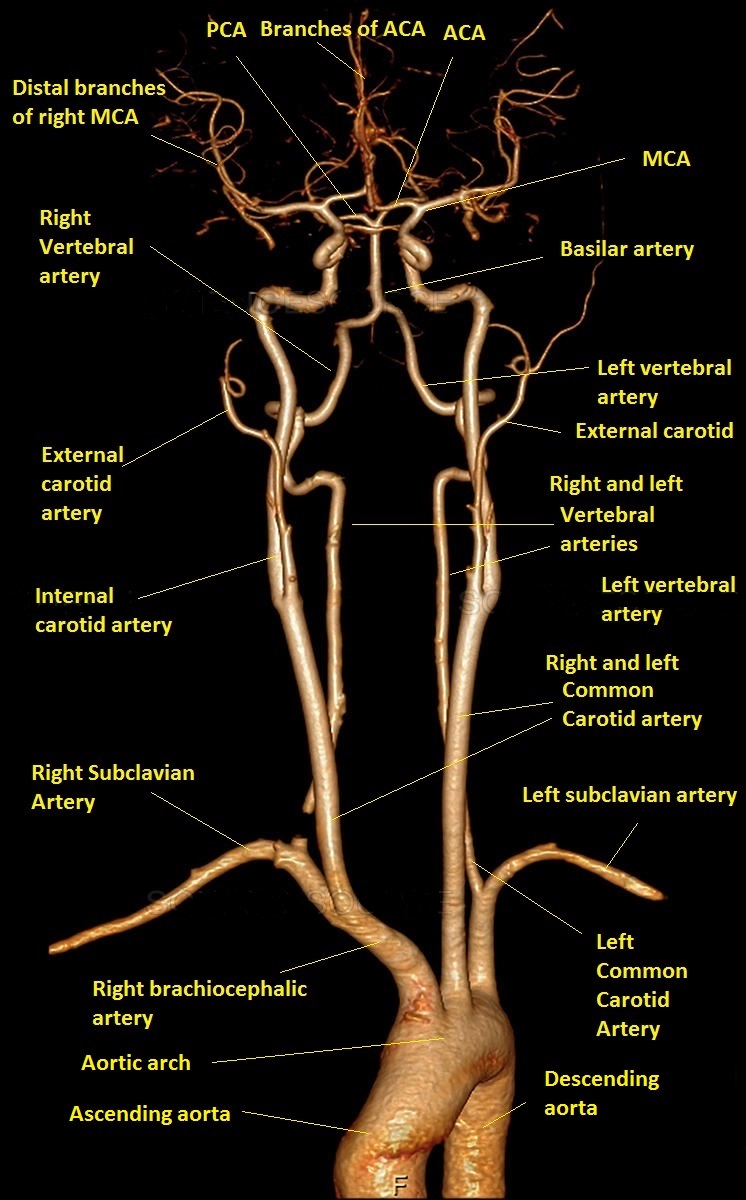
🩻 CT Angiography (CTA)
- 💡 Provides rapid 3D vascular imaging using iodinated contrast and CT reconstruction.
- ⚡ Excellent for detecting large vessel occlusion (LVO) in acute stroke → guides thrombectomy.
- 📈 Almost as accurate as DSA for extracranial stenosis and highly accurate for intracranial stenosis and dissection.
- 🚫 Avoid or use cautiously in contrast allergy or renal impairment — check eGFR.
- ⚠️ Carries radiation exposure; uses iodine-based contrast that can cause nephrotoxicity.
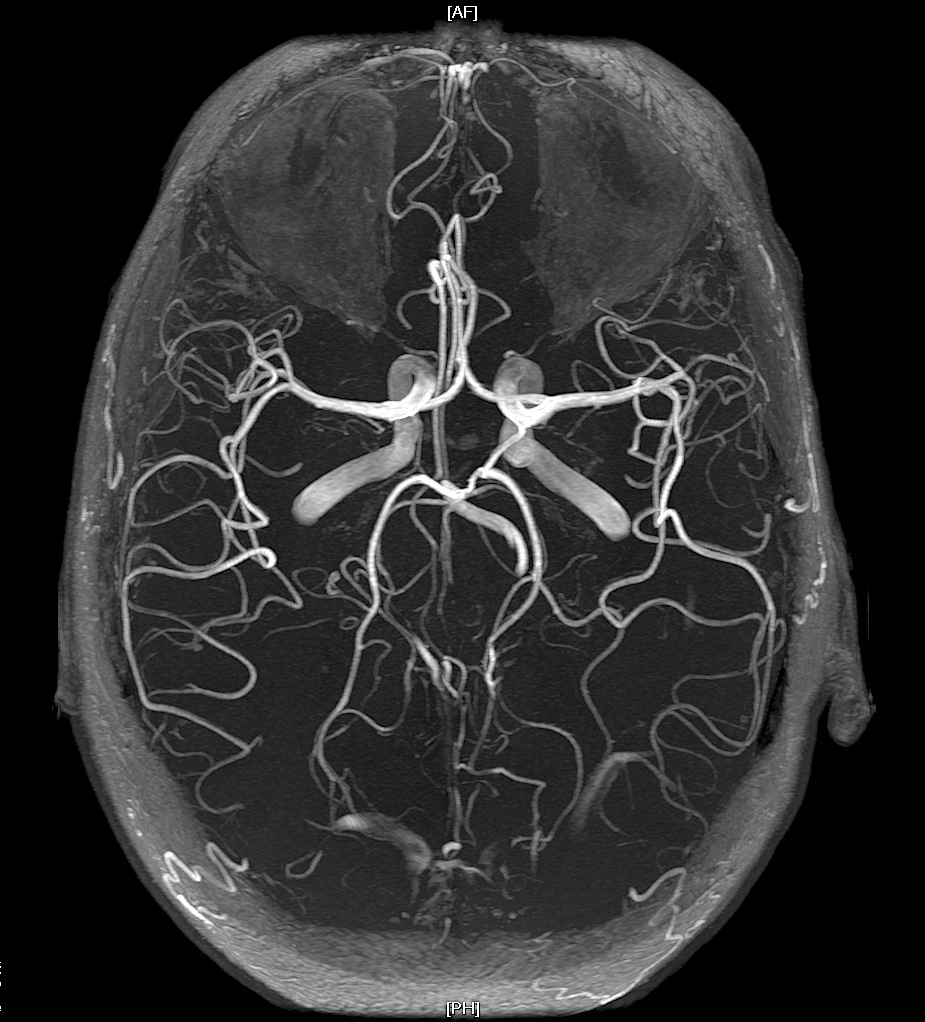
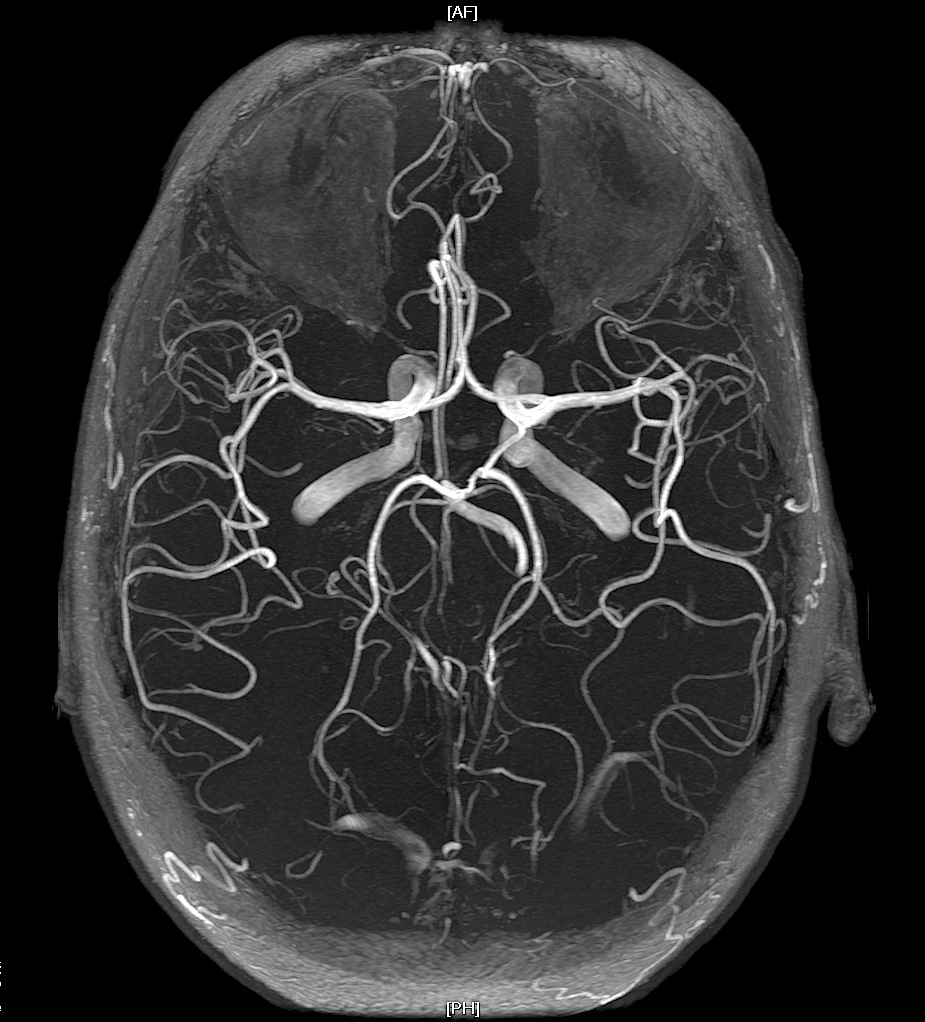
🧲 MR Angiography (MRA)
- 🧠 Non-invasive imaging of cerebral vasculature using blood flow signal differences.
Can be done without contrast (TOF or phase-contrast) or with gadolinium contrast.
- Time-of-Flight (TOF): Flow-dependent, uses inflow enhancement of unsaturated blood — good for arteries, may overestimate stenosis.
- Phase-Contrast (PC): Uses velocity phase shifts — good for both arteries and veins, often used for cardiac/aortic studies.
- Contrast-Enhanced MRA (CE-MRA): Gadolinium shortens T1 relaxation, producing high intravascular signal and excellent vessel definition.
- ⚠️ Risks: Gadolinium reactions, nephrogenic systemic fibrosis (rare, CKD), and slight overestimation of stenosis.
- ✅ Accuracy similar to DSA for many cerebral indications; faster and safer for routine use.
🩸 CT Venography (CTV)
CTV assesses venous anatomy and patency and can be combined with CTA for dual arterial-venous imaging.
Particularly useful in suspected Cerebral Venous Thrombosis (CVT) — shows sinus filling defects and collateral drainage.
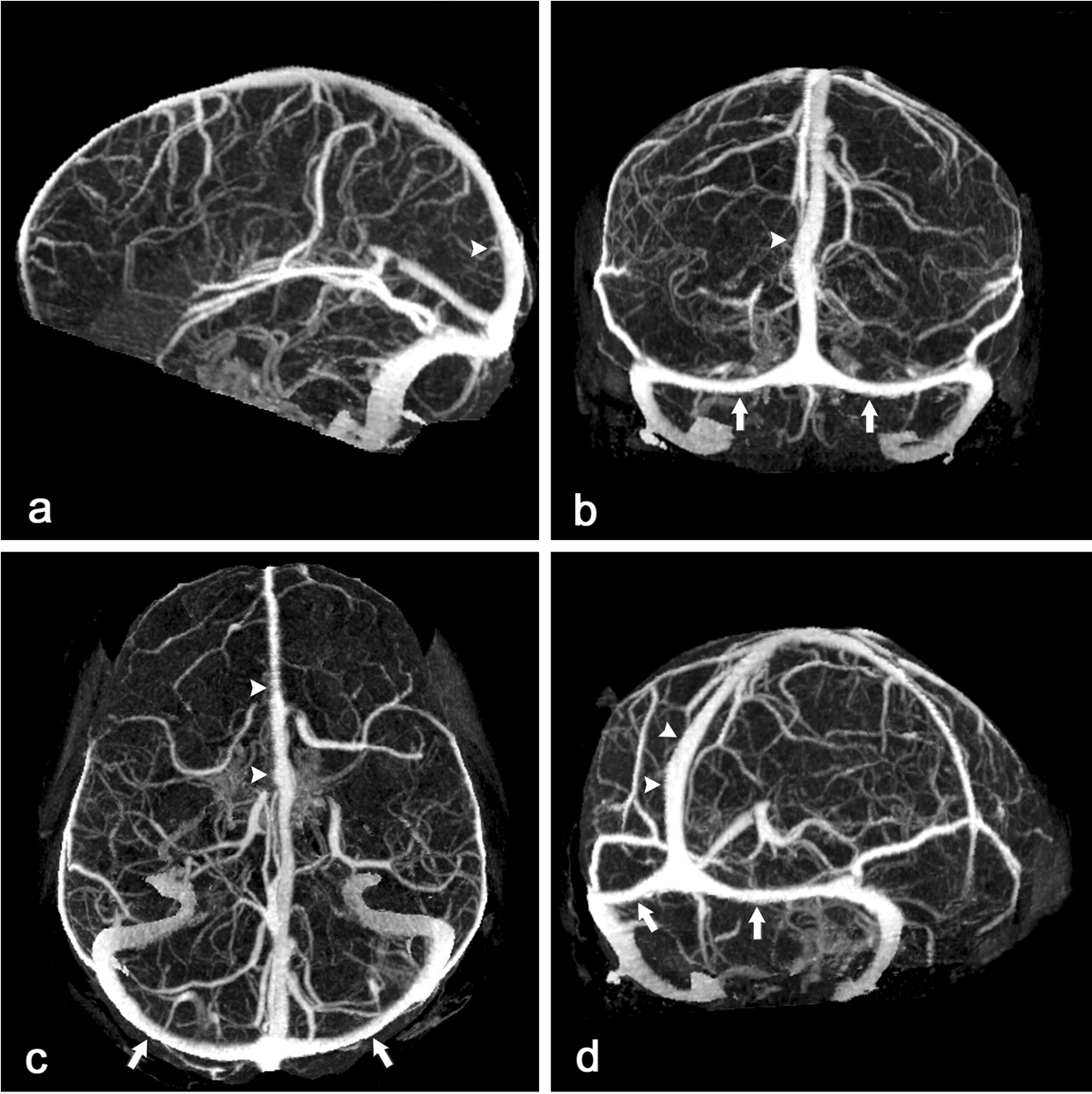
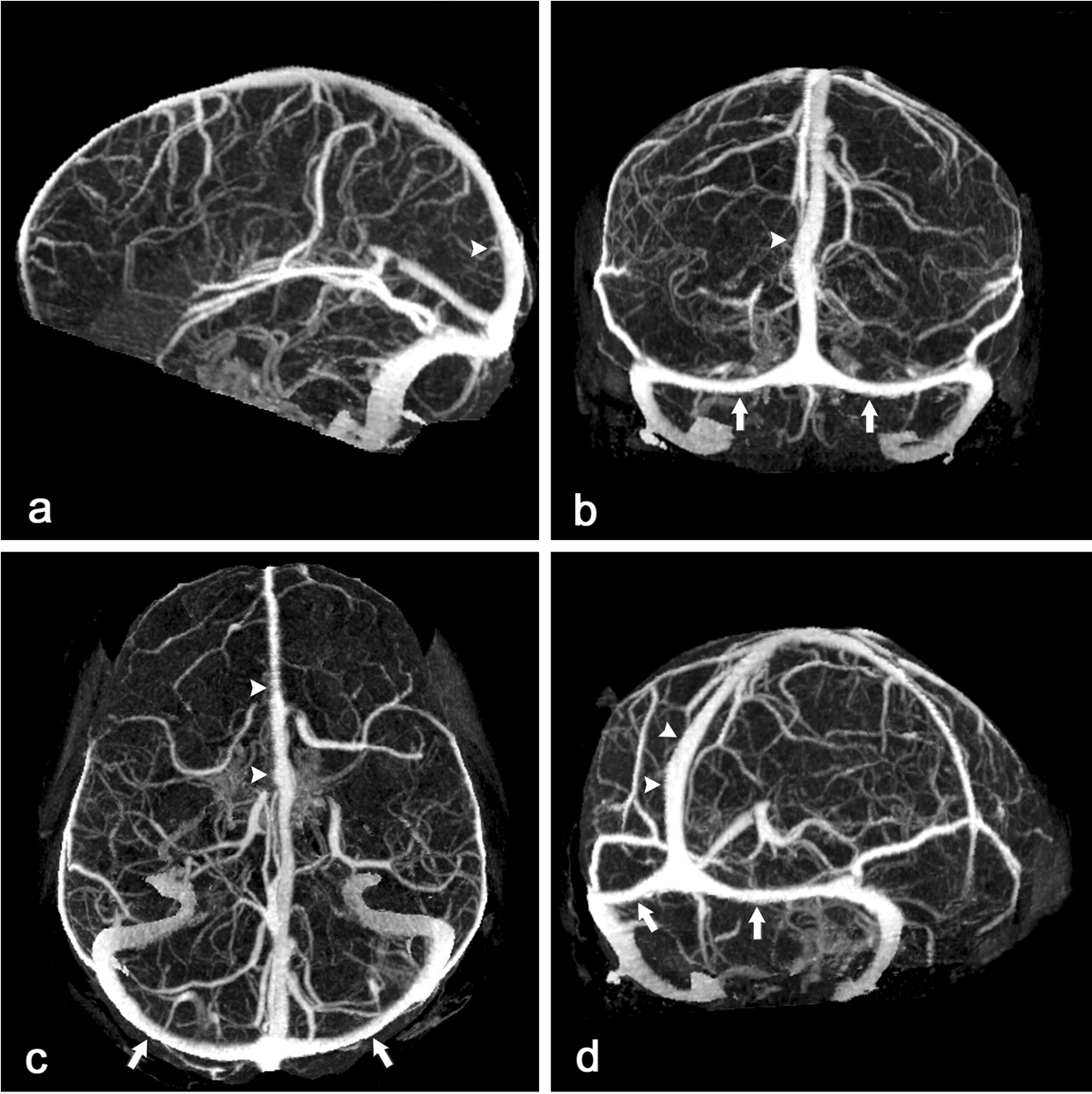
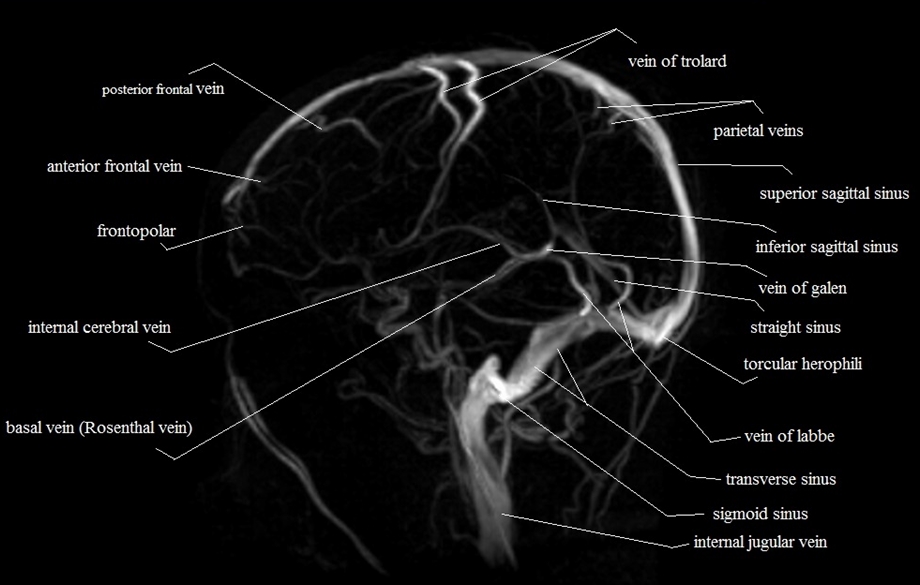
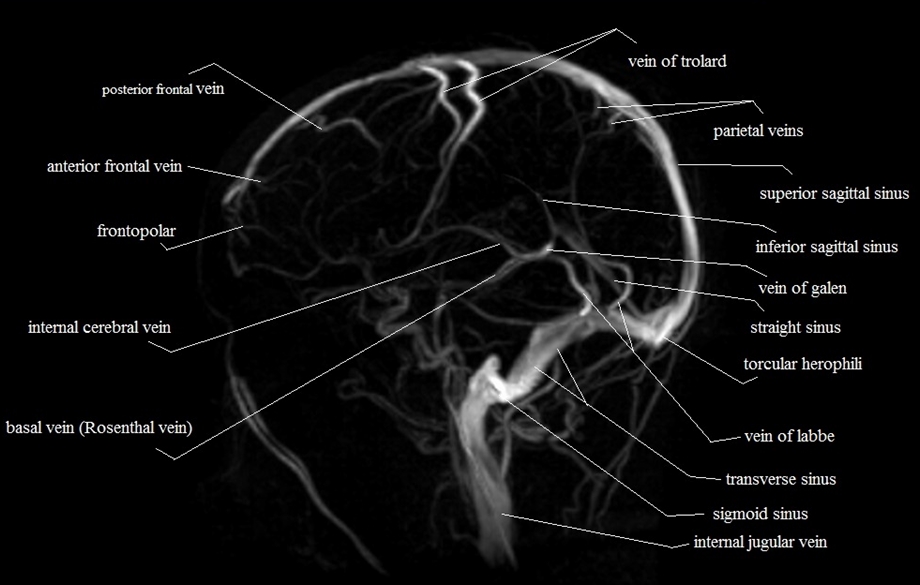
🧲 MR Venography (MRV)
Investigation of choice in suspected CVT. Demonstrates absence of flow or intraluminal thrombus in dural venous sinuses.
Can be performed non-contrast TOF or contrast-enhanced for better delineation.
🔎 Angiographic Findings
| 🧩 Aetiology | 🔬 Typical Finding |
|---|
| Aneurysm | Focal balloon-like outpouching of vessel wall. |
| Dissection | Smooth tapering (“string sign”), double lumen, or intimal flap; may progress to pseudoaneurysm or occlusion. |
| Vasculitis | Segmental narrowing and dilation → “beading” pattern, especially in medium-sized arteries. |
| Takayasu’s / Moyamoya | Multiple collaterals (“puff of smoke” appearance) from anastomotic vessels. |
🧬 Causes of “Beading” Appearance
| 🧠 Possible Causes |
|---|
- Cerebral vasculitis (primary or secondary)
- Tumour embolisation
- Radiation-induced vasculopathy
- Meningitis / chronic meningitis
- Cocaine or amphetamine use
- Reversible cerebral vasoconstriction syndrome (RCVS)
- Malignant intravascular lymphoma
- Fabry’s disease
- Phaeochromocytoma
|
💡 Teaching tip:
- DSA remains gold standard for intervention planning.
- CTA excels for acute stroke triage and dissections.
- MRA/MRV preferred when radiation or iodine contrast contraindicated.
- Beading = think vasculitis, RCVS, or sympathomimetic drugs.