| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Bacterial Meningitis in Children
Related Subjects: |Acute Epiglottitis |Croup |Acute Tracheitis |Stridor |Acute Bacterial Meningitis in Children |Pneumonia in Children |Cystic Fibrosis |Sweat Test |Encopresis in Children |Enuresis/Bedwetting in Children |Acute Glomerulonephritis in Children |Nephrotic Syndrome in Children |Acute Appendicitis in Children |Gastro-oesophageal reflux in Children |Intussusception in Children |Panayiotopoulos Syndrome in Children |Reflex anoxic attacks in Children |Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections
🧠 Introduction
Meningococcal disease remains the leading cause of meningitis in children across the UK and Ireland, claiming more lives under five than any other infectious illness. Even survivors may face lifelong consequences including hearing loss, seizures, limb amputation, or neurocognitive and behavioural difficulties. Prompt recognition and urgent management save lives.
💉 Acute Bacterial Meningitis in Children
- Acute bacterial meningitis is a medical emergency involving infection of the meninges — the protective membranes surrounding the brain and spinal cord.
- It can progress rapidly from fever and malaise to shock, coma, and death within hours if untreated.
- Early empirical antibiotic therapy, ideally within the first hour of suspicion, is essential.
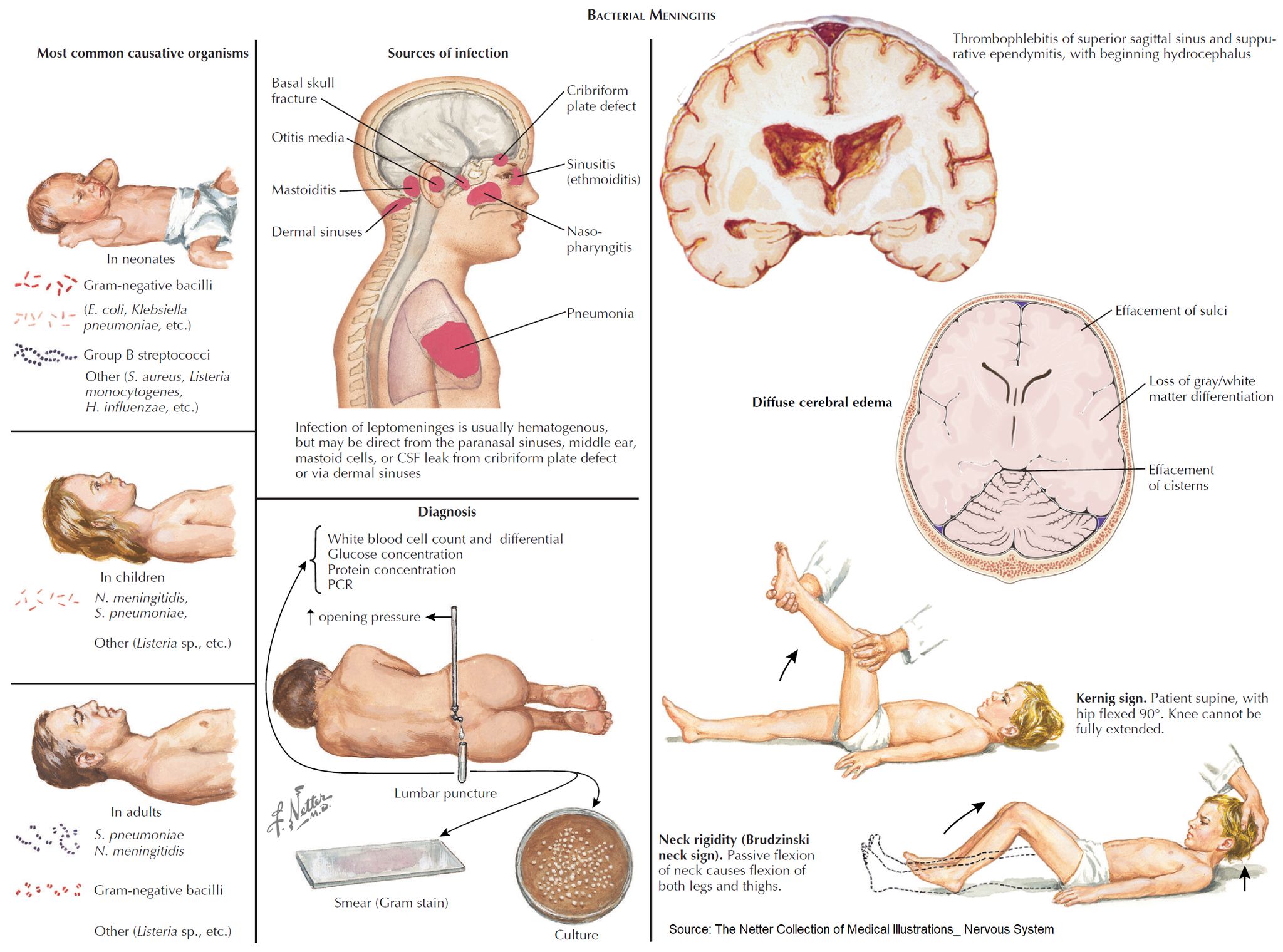
🦠 Common Causative Organisms
- Neisseria meningitidis (meningococcus) — leading cause in children and adolescents.
- Streptococcus pneumoniae (pneumococcus).
- Haemophilus influenzae type b (Hib) — now rare due to vaccination.
- Group B Streptococcus — common in neonates (transmitted during labour).
- Listeria monocytogenes — in neonates or immunocompromised children.
🧪 The Tumbler Test
Press a clear glass tumbler firmly against the rash. If the rash does not fade and remains visible through the glass, this is a sign of meningococcal septicaemia — call 999 or seek emergency help immediately. Check the entire body, including lighter skin areas (palms, soles, eyelids, roof of mouth). Rashes may start as tiny red or brown pinpricks and evolve into larger purpuric or hemorrhagic lesions.

⚠️ Symptoms & Clinical Features
- High fever ≥38°C, chills, nausea, vomiting.
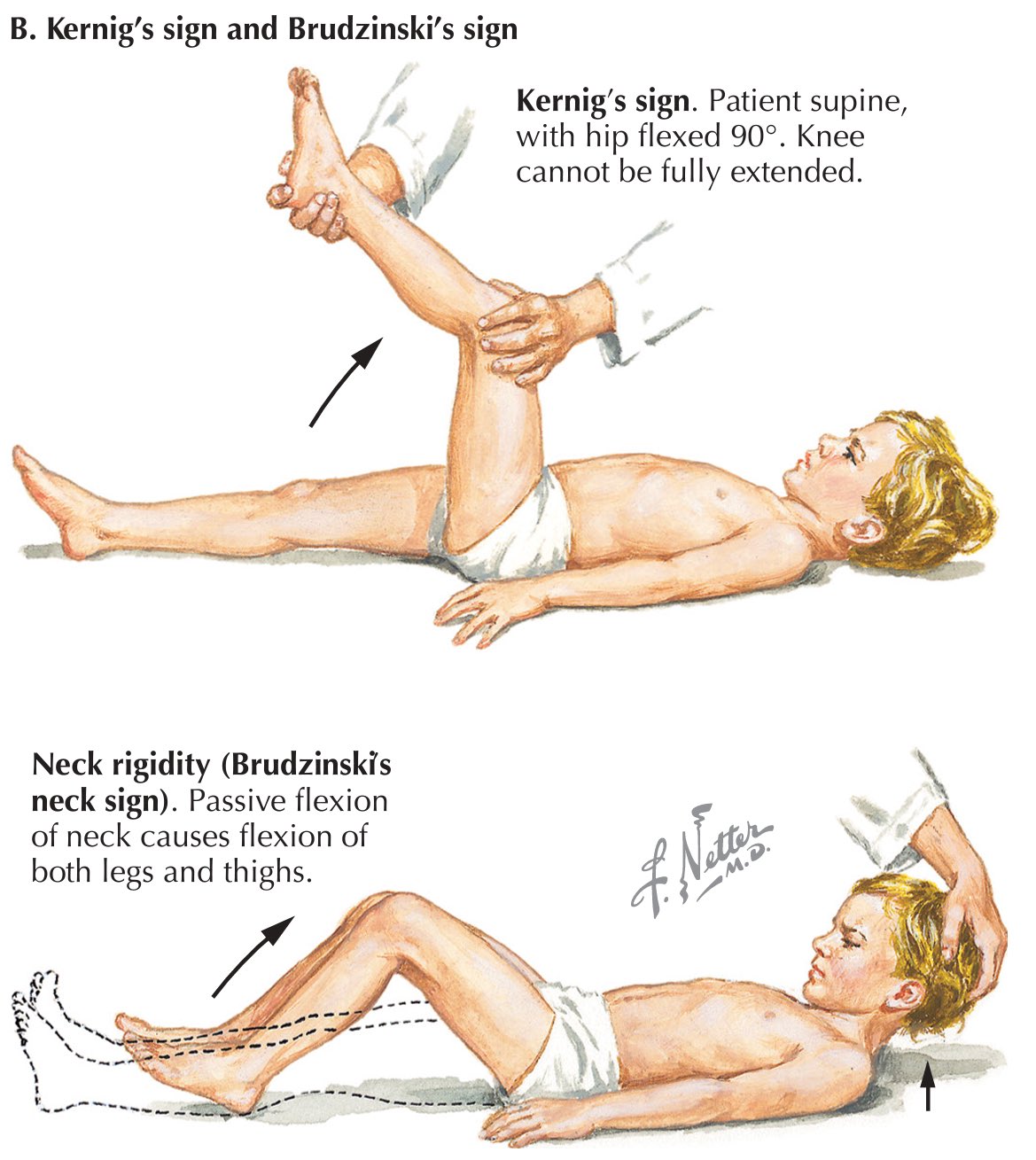
- Severe headache and neck stiffness.
- Non-blanching rash (purpuric or petechial).
- Photophobia and altered mental state or irritability.
- Cold extremities, tachypnoea, or mottled skin (suggests sepsis).
- Myalgia, limb pain, or refusal to walk in children.
- In infants: poor feeding, high-pitched cry, lethargy, bulging fontanelle, hypotonia or stiffness, seizures, or unresponsiveness.
🚨 Do not wait for classical meningeal signs — meningococcal disease often presents with fever, lethargy, and vomiting before rash or photophobia. If in doubt, treat empirically and refer urgently.
🔬 Diagnosis
- Blood tests: FBC, U&E, CRP, blood culture, and lactate.
- Microbiology: Nasopharyngeal swab, urine, and stool if indicated; PCR for Neisseria and Streptococcus species.
- Lumbar puncture (LP): Once safe (no raised ICP). Collect 3 bottles:
- 1 – Gram stain & culture.
- 2 – Glucose, protein (compare to plasma glucose).
- 3 – PCR/virology.
- Imaging (CT/MRI): Before LP if focal deficits or papilloedema present.
💊 Pre-Hospital Emergency Antibiotics (UK)
- 💉 Benzylpenicillin IM: Give immediately if meningococcal disease suspected, unless delay will impede transfer.
- Up to 1 year: 300 mg IM
- 1–9 years: 600 mg IM
- ≥10 years: 1.2 g IM
- Allergic to penicillin → Cefotaxime 50 mg/kg IM (max 1 g if >12 yrs).
- Document rationale if pre-hospital antibiotics were not given.
🏥 In-Hospital Antibiotic Therapy
Start IV antibiotics immediately — do not delay for LP or imaging. Always check local paediatric sepsis guidelines and adjust for age/weight.
- Ceftriaxone 50–80 mg/kg/day (max 2–4 g) if >3 months old or Cefotaxime 50 mg/kg q6–8h if <3 months.
- Vancomycin – add for suspected or proven resistant pneumococci.
- Ampicillin – add in neonates and immunocompromised for Listeria and Group B strep.
- HIV-positive children: consider Cryptococcus coverage if indicated.
- Listeria: treat with IV ampicillin + gentamicin; microabscesses and pneumonia may occur in neonates.
💉 Adjunctive & Supportive Care
- Fluids & electrolytes: Maintain perfusion but avoid fluid overload (risk of cerebral oedema).
- Dexamethasone 0.15 mg/kg IV q6h × 4 days — start with first antibiotic dose if >3 months and H. influenzae suspected (not for meningococcal sepsis).
- Seizure control: Use benzodiazepines or levetiracetam if recurrent.
- Monitor: HR, BP, SpO₂, temperature, neurological status, urine output.
- PICU care: Consider for shock, respiratory failure, or raised ICP.
- Inotropes: dopamine or dobutamine 10 mcg/kg/min (can run peripherally). If escalating to adrenaline, use central access (0.1 mcg/kg/min).
- Advanced therapies (specialist centres): ECMO, protein C concentrate, heparin for DIC, or plasmapheresis for cytokine storm (experimental).
🛡️ Prevention
- Routine vaccination — Hib, meningococcal (MenB, MenACWY), and pneumococcal vaccines.
- Good hygiene and respiratory etiquette.
- Prophylaxis for close contacts: Rifampicin or ciprofloxacin within 24 h of exposure to confirmed meningococcal disease.
📈 Prognosis & Complications
- Mortality: up to 10% even with optimal care.
- Sequelae: hearing loss, cognitive deficits, epilepsy, hydrocephalus, subdural effusion, or limb loss from necrosis.
- Early steroids and rapid antibiotics reduce risk of deafness and neurological impairment.
💡 Key Learning Point: In any febrile child who looks unwell, consider meningococcal sepsis until proven otherwise. Early recognition and antibiotics — even before confirmation — save lives.
