Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Blood Pressure
Blood pressure (BP) is the pressure of blood within the arterial system. It is vital to maintain perfusion of the brain, heart and other organs, but both too high and too low can cause harm. This article covers:
- What blood pressure is and how it is generated.
- How BP is controlled (neural, hormonal & renal mechanisms).
- Hypotension – causes, clinical features and principles of management.
- Hypertension – pathophysiology, complications and key concepts.
1️⃣ What Is Blood Pressure?
Blood pressure is the force exerted by blood on the walls of arteries. It is usually expressed as:
- Systolic BP (SBP): peak pressure during ventricular systole (LV contraction).
- Diastolic BP (DBP): minimum pressure during ventricular diastole (LV relaxation).
The arterial circulation is not a rigid pipe; it is a compliant, branching tree. As blood flows from the aorta through arteries → arterioles → capillaries → veins, pressure falls progressively.
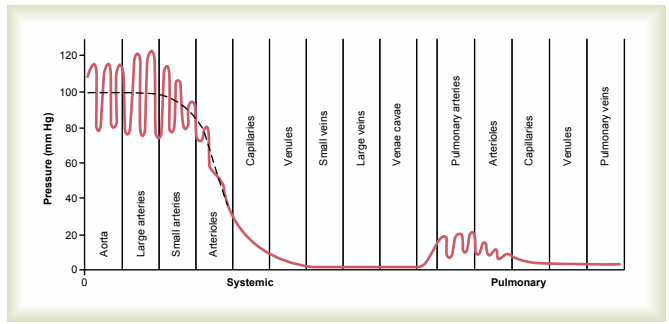
💡 The biggest pressure drop occurs across the arterioles. They are the main site of resistance and therefore the primary regulators of systemic vascular resistance (SVR) – the “taps” of the circulation.
At a simple level:
Mean Arterial Pressure (MAP) ≈ Cardiac Output (CO) × Systemic Vascular Resistance (SVR)
- CO = HR × Stroke Volume (how much blood the heart pumps).
- SVR is set mainly by arteriolar tone (constriction vs dilation).
2️⃣ Neural, Hormonal & Renal Control of Blood Pressure
BP is tightly controlled by fast neural reflexes and slower hormonal and renal mechanisms.
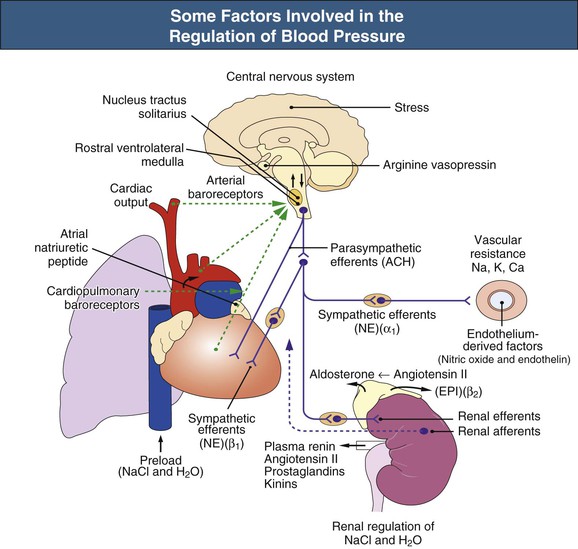
Neural Control
- Baroreceptors:
- Located in the carotid sinus & aortic arch.
- Sense vessel wall stretch and relay signals to the brainstem (NTS).
- ⬆️ BP → ⬆️ stretch → ⬆️ baroreceptor firing → reflex ⬇️ sympathetic and ⬆️ parasympathetic outflow → ↓ HR & SVR.
- Sympathetic nervous system:
- ⬆️ HR (positive chronotropy).
- ⬆️ contractility (inotropy).
- ⬆️ arteriolar vasoconstriction (↑ SVR).
- Parasympathetic (vagal) tone:
- Acts mainly on the heart → ⬇️ HR and modest ↓ cardiac output.
- Little direct effect on systemic arteriolar tone.
Hormonal Control
- RAAS (Renin–Angiotensin–Aldosterone System):
- Renin released from JG cells in kidney (low BP, low Na⁺, sympathetic activation).
- Renin converts angiotensinogen → Ang I → Ang II (via ACE).
- Ang II: potent vasoconstrictor (↑ SVR) + stimulates aldosterone.
- Aldosterone: increases Na⁺ and water reabsorption in distal nephron → ↑ blood volume → ↑ BP.
- ADH (vasopressin):
- Released from posterior pituitary in response to high osmolality or low BP.
- ⬆️ water reabsorption in collecting ducts + vasoconstriction → ↑ BP.
- ANP / BNP:
- Released when atria/ventricles are stretched.
- Promote natriuresis and vasodilation → ⬇️ blood volume and BP.
Renal Control (Long-Term)
- Kidneys set the long-term “BP thermostat” via sodium and water balance.
- Chronic hypertension reflects a shifted pressure–natriuresis relationship – the kidney only excretes enough salt and water at a higher BP.
- Most antihypertensive strategies ultimately work by altering this kidney–pressure relationship.
3️⃣ Hypotension (Low Blood Pressure)
There is no single universal cut-off, but hypotension usually refers to:
- SBP <90 mmHg or MAP <65 mmHg with symptoms or organ hypoperfusion.
- In practice: any BP lower than the patient’s normal, associated with dizziness, syncope, confusion, oliguria or shock.
Types & Causes of Hypotension
- Absolute hypotension: BP genuinely low.
- Hypovolaemic: haemorrhage, vomiting/diarrhoea, burns, over-diuresis.
- Cardiogenic: MI, severe heart failure, arrhythmias, valvular disease.
- Distributive: sepsis, anaphylaxis, neurogenic shock (loss of sympathetic tone).
- Endocrine: adrenal crisis, hypothyroidism (RARE as primary driver alone).
- Relative hypotension: BP may be “normal” by numbers but too low for that patient (e.g. long-standing hypertensive whose SBP falls from 190 → 120 mmHg and becomes confused).
- Orthostatic (postural) hypotension:
- Drop in SBP ≥20 mmHg or DBP ≥10 mmHg within 3 minutes of standing.
- Causes: autonomic failure, volume depletion, drugs (α-blockers, nitrates, diuretics, antidepressants).
Clinical Features of Hypotension
- Dizziness, light-headedness, blurred vision.
- Syncope or near-syncope.
- Cold clammy peripheries, prolonged capillary refill in shock.
- Oliguria, confusion, chest pain, dyspnoea – signs of organ hypoperfusion.
Principles of Management (High-Level)
- 🔎 Identify cause: history, exam, ECG, bloods, CXR, bedside echo if available.
- 🧪 Assess for shock: lactate, urine output, mentation, skin perfusion.
- 💧 Volume resuscitation if hypovolaemic or distributive (balanced crystalloids, blood if haemorrhage).
- ❤️ Inotropes/vasopressors (e.g. norepinephrine) in shock under critical care guidance.
- 🧠 Drug review: pause or adjust antihypertensives, nitrates and other BP-lowering agents if contributing.
- 📐 Orthostatic hypotension: hydration, slow posture changes, compression stockings, review drugs; specialist treatments (e.g. fludrocortisone, midodrine) in selected patients.
💡 Low BP only matters if it causes poor perfusion. Some young, fit people have SBP 90–100 and feel well – this can be normal for them.
4️⃣ Hypertension (High Blood Pressure)
Hypertension is sustained elevation of arterial blood pressure. Definitions vary slightly between guidelines, but in clinic adults are generally considered hypertensive if:
- Clinic BP is ≥140/90 mmHg, confirmed by:
- Ambulatory BP monitoring (ABPM) or
- Home BP monitoring (HBPM) averages.
Primary vs Secondary Hypertension
- Primary (essential) hypertension:
- ~90–95% of cases.
- Multifactorial: genetics, age, obesity, salt intake, RAAS and sympathetic overactivity, reduced NO, vascular stiffness.
- Secondary hypertension: due to an identifiable cause:
- Renal parenchymal disease, renovascular disease (RAS).
- Endocrine: primary hyperaldosteronism, phaeochromocytoma, Cushing’s, hyperthyroidism, acromegaly.
- Coarctation of the aorta.
- Drugs: NSAIDs, steroids, ciclosporin, OCP, sympathomimetics, liquorice.
Why Hypertension Matters – Target Organ Damage
Chronic high BP damages blood vessels and organs over years:
- 🧠 Brain: lacunar infarcts, intracerebral haemorrhage, vascular dementia.
- ❤️ Heart: LV hypertrophy, coronary artery disease, MI, heart failure, AF.
- 🩺 Kidneys: nephrosclerosis, chronic kidney disease, proteinuria.
- 👁️ Eyes: hypertensive retinopathy (AV nipping, haemorrhages, exudates, papilloedema).
- 🦵 Peripheral vasculature: peripheral arterial disease, aneurysms, dissections.
💡 For teaching: think “brain, heart, kidneys, eyes, vessels” whenever you see long-standing hypertension.
5️⃣ Measuring Blood Pressure Properly (Clinical Corner)
Correct measurement is essential to avoid mislabelling patients. Key steps:
- 🧘 Prepare: Patient seated 5 minutes, feet flat, legs uncrossed, arm supported at heart level.
- 🩹 Cuff size: ensure the bladder covers ≥80% of arm circumference; too small → false high, too large → false low.
- 🫀 Technique:
- Palpate radial artery, inflate cuff until pulse disappears to estimate SBP.
- Place stethoscope over brachial artery, inflate 20–30 mmHg above estimate.
- Deflate slowly (~2 mmHg/sec) and listen for Korotkoff sounds:
- Phase I: first tapping = systolic.
- Phase V: disappearance = diastolic (use Phase IV “muffling” if sounds persist to zero).
- 📝 Record: SBP/DBP, arm, position, device; take ≥2 readings and average. Measure both arms at least once.
6️⃣ Pulse Pressure, Arm Differences & Special Patterns
- Pulse pressure = SBP − DBP
- Narrow pulse pressure: aortic stenosis, severe LV failure, shock.
- Wide pulse pressure: aortic regurgitation, PDA, severe thyrotoxicosis, high-output states.
- Arm–arm BP difference:
- Persistent >15–20 mmHg difference suggests subclavian stenosis or dissection.
- Small 5–10 mmHg differences are common and usually benign.
- Arm vs ankle: lower ankle pressure suggests peripheral arterial disease or coarctation (low leg BP, radio–femoral delay).
7️⃣ Overview of Management Principles
Hypertension – Big Picture
- Confirm with ABPM/HBPM rather than a single clinic reading.
- Assess global CV risk (age, sex, smoking, diabetes, lipids, family history).
- Look for target organ damage (CKD, LVH, retinopathy, prior stroke/MI).
- Start with lifestyle:
- Weight loss, salt restriction, exercise, alcohol moderation, smoking cessation, sleep hygiene.
- Add drug therapy as indicated (ACEi/ARB, CCB, thiazide-type diuretic, etc.), titrating to appropriate targets and monitoring U&Es and BP.
📊 Current Blood Pressure Guidelines – Quick Reference
🇬🇧 UK (NICE NG136 – 2025 visual summary)
Clinic (office) BP vs ABPM/HBPM, plus treatment targets.
| Category / Context | Clinic (office) BP | ABPM / HBPM (average) | Notes (Adults ≥18 years) |
|---|---|---|---|
| Normal BP | 90/60 to <140/90 mmHg | <135/85 mmHg | No hypertension diagnosis; advise on healthy lifestyle. |
| Threshold for HTN diagnosis | ≥140/90 mmHg | ≥135/85 mmHg | Confirm diagnosis with ABPM (preferred) or HBPM.:contentReference[oaicite:0]{index=0} |
| Stage 1 Hypertension | 140/90–159/99 mmHg | Daytime average 135/85–149/94 mmHg | Offer lifestyle advice to all; start drugs if <80 with ≥10% 10-yr CVD risk, target organ damage, CKD, diabetes, or any ≥80 with clinic BP >150/90.:contentReference[oaicite:1]{index=1} |
| Stage 2 Hypertension | ≥160/100 mmHg (up to 179/119) | ≥150/95 mmHg | Offer drug treatment to all, plus lifestyle advice.:contentReference[oaicite:2]{index=2} |
| Severe HTN / Possible emergency | ≥180 systolic or ≥120 diastolic | — | Same-day specialist assessment, especially if symptoms or target organ damage (e.g. retinal haemorrhages, papilloedema, encephalopathy, AKI).:contentReference[oaicite:3]{index=3} |
| Low BP (hypotension – general NHS definition) | ≤89/59 mmHg | — | May be normal in young fit adults; clinically important if symptomatic or with organ hypoperfusion.:contentReference[oaicite:4]{index=4} |
| Treatment target <80 years | <135/85 mmHg (equivalent office target) | <135/85 mmHg | Aim for <135/85 if tolerated, whether or not established CVD.:contentReference[oaicite:5]{index=5} |
| Treatment target ≥80 years | <145/85 mmHg | <145/85 mmHg | Use clinical judgement & frailty; avoid overtreatment but don’t ignore very high readings.:contentReference[oaicite:6]{index=6} |
💡 In UK practice: diagnose HTN at clinic ≥140/90 confirmed by ABPM/HBPM ≥135/85; treat to <135/85 (<80 yrs) or <145/85 (≥80 yrs) if tolerated.
🌍 International BP Classifications (Office Readings)
Useful for comparing UK, European (ESH) and US (ACC/AHA) schemes.
| Category | UK / NICE (diagnosis focus) | 2023 ESH (Europe) – Office BP:contentReference[oaicite:7]{index=7} | 2017 ACC/AHA (US) – Office BP:contentReference[oaicite:8]{index=8} |
|---|---|---|---|
| Normal | Roughly <140/90 mmHg in clinic; normal range often quoted as 90/60–120/80.:contentReference[oaicite:9]{index=9} | <130/85 mmHg (includes “optimal” <120/80 and “normal” 120–129/<80) | <120/<80 mmHg |
| High-normal / Elevated | No formal “elevated” band; 120–139/80–89 often considered “high-normal” but not labelled separately in NG136. | High-normal: 130–139 and/or 85–89 mmHg | Elevated: 120–129 and <80 mmHg |
| Grade 1 / Stage 1 HTN | Stage 1: 140/90–159/99 mmHg (confirm with ABPM/HBPM ≥135/85).:contentReference[oaicite:10]{index=10} | Grade 1: 140–159 and/or 90–99 mmHg | Stage 1: 130–139 or 80–89 mmHg (diagnosis threshold ≥130/80) |
| Grade 2 / Stage 2 HTN | Stage 2: ≥160/100 mmHg (up to 179/119). | Grade 2: 160–179 and/or 100–109 mmHg | Stage 2: ≥140 or ≥90 mmHg |
| Grade 3 / Severe HTN | Often described as “severe” at ≥180 systolic or ≥120 diastolic; treat urgently and consider emergency if symptomatic.:contentReference[oaicite:11]{index=11} | Grade 3: ≥180 and/or ≥110 mmHg | Falls within Stage 2 but flagged as hypertensive crisis if ≥180/120 or with acute end-organ damage. |
Hypotension – Big Picture
- Always treat the cause (bleeding, sepsis, MI, arrhythmia, drugs, dehydration).
- Support circulation (positioning, fluids, vasopressors/inotropes where needed).
- For postural hypotension, review medications, optimise volume status, and teach physical counter-manoeuvres.
8️⃣ Summary
- Blood pressure reflects the interaction between cardiac output and systemic vascular resistance.
- Arterioles are the key resistance vessels and the site of the largest pressure drop.
- BP is controlled by rapid neural mechanisms, slower hormones (RAAS, ADH, ANP) and long-term renal regulation.
- Hypotension matters when it impairs organ perfusion – think cause and shock.
- Hypertension is a chronic vascular risk factor causing stroke, MI, CKD and more; meticulous control prevents end-organ damage.
- Accurate measurement and thoughtful interpretation are the starting point for every good BP consultation.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology