| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Diabetic Ketoacidosis (DKA) Children
🩺 Initial Assessment
- 📝 History & Exam: Look for vomiting 🤮, abdominal pain, dehydration (dry lips, sunken eyes), lethargy 💤, and deep breathing (Kussmaul respiration 🫁). Check for infection as a precipitating factor.
- ❤️ Vital Signs: Record heart rate, respiratory rate, BP, capillary refill, oxygen saturation, and temperature 🌡️.
- 💡 Key point: DKA can mimic sepsis → always think about dual pathology.
📖 BSPED Guideline
- UK guideline follows ISPAD definition: pH <7.3 or HCO₃ <15 mmol/L with ketones >3.0 mmol/L = DKA ✅
📊 BSPED Severity Classification
- 🟢 Mild: pH 7.2–7.29 or HCO₃ <15 → assume 5% dehydration.
- 🟠 Moderate: pH 7.1–7.19 or HCO₃ <10 → assume 5% dehydration.
- 🔴 Severe: pH <7.1 or HCO₃ <5 → assume 10% dehydration.
💡 Clinical Pearl: Careful, gradual rehydration is essential ⚖️ – too rapid fluids ↑ risk of cerebral oedema. But shock = resuscitate first.
🔎 Investigations
- 🧪 Bloods: Glucose, VBG/ABG (pH, HCO₃), Na⁺, K⁺, urea, creatinine.
- 💧 Urine: Dip for ketones.
- 🦠 Infection screen: CXR, cultures if infection suspected.
- ⚡ ECG: Monitor potassium (peaked T waves in hyperkalaemia, flattened T in hypokalaemia).
⚡ Initial Management
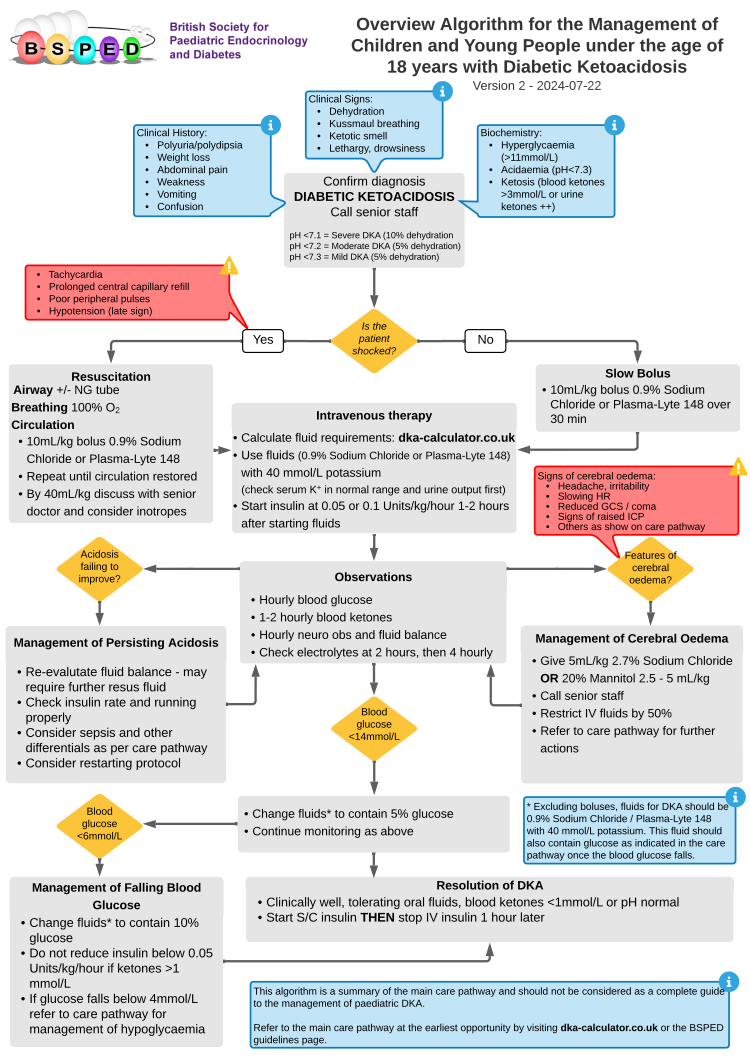
- 🫁 Airway: Ensure patency. Insert airway if comatose. NG tube if reduced consciousness to prevent aspiration.
- 💨 Breathing: Give 100% O₂ if hypoxic. Watch for Kussmaul breathing.
- 💓 Circulation: Insert IV access, monitor BP/HR, start cardiac monitoring.
- 💉 Shocked child: Give 10 ml/kg 0.9% NaCl bolus 💧 (repeat if persistent shock). Discuss with senior/ICU early.
- 💧 Not shocked: Give 10 ml/kg 0.9% NaCl over 30 min (some centres use PlasmaLyte).
- 💊 Insulin: Start low-dose infusion after fluids (0.05–0.1 units/kg/hr). ❌ No bolus.
- ⚡ Potassium: Replace once U&E available – insulin drives K⁺ into cells → risk of hypokalaemia ⚠️.
- 👀 Monitoring: Check glucose, ketones, electrolytes, gases every 1–2 hrs. Perform neuro checks for cerebral oedema.
- 🦠 Treat triggers: Infections, missed insulin, new diabetes diagnosis.
- 🍽️ Transition: When ketones cleared + child eating, switch to SC insulin.
- 📚 Education: Teach family about diabetes care, sick day rules, and recognising early DKA signs.
☠️ Causes of Death in DKA
- 🧠 Cerebral oedema: Most feared complication. Often in young/newly diagnosed children. Mortality ~25%.
- ⚡ Hypokalaemia: Preventable with careful replacement.
- 🌬️ Aspiration pneumonia: Use NG tube if vomiting or reduced consciousness.
- 💔 Inadequate resuscitation: Poor perfusion worsens brain injury risk. Always treat shock aggressively.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
