Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Myelodysplastic syndrome (Myelodysplasia)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Iron deficiency Anaemia
|Haemolytic anaemia
|Macrocytic anaemia
|Megaloblastic anaemia
|Microcytic anaemia
|Myelodysplasia
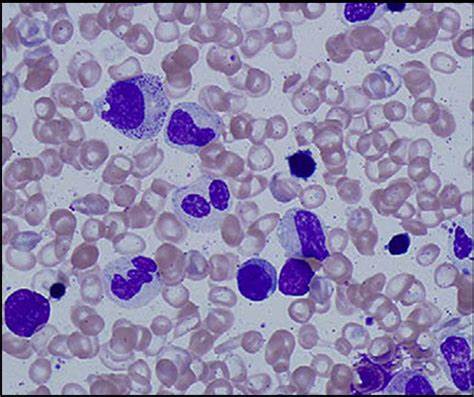
🧬 Malignant haematological condition characterised by ineffective haematopoiesis, cytopenias, and a risk of transformation into acute myeloid leukaemia (AML).
Key Point: Median survival is < 2 years in many subtypes, with infection and bleeding being the most common causes of death. ⚠️
📖 About
🧬 Aetiology
👶 Commoner in association with:
📊 WHO Classification of MDS
Disease Bone marrow findings
MDS with single-lineage dysplasia < 5% blasts; dysplasia confined to one lineage
MDS with ring sideroblasts (MDS-RS) >15% ring sideroblasts, or 6–14% with SF3B1 mutation
MDS with multilineage dysplasia < 5% blasts; dysplasia in ≥2 lineages
MDS with excess blasts 5–19% blasts
MDS with isolated del(5q) < 5% blasts; del(5q) cytogenetic abnormality; often ↑ platelets
MDS, unclassifiable Does not fit above categories or inadequate marrow material
🩺 Clinical Features: Progressive Bone Marrow Failure
🔍 Investigations
💊 Management (Prognosis often poor)
📚 References
Cases — Myelodysplastic Syndrome (MDS)
- Case 1 — Incidental Cytopenia in Elderly: A 76-year-old man is found to have anaemia on a routine check (Hb 9.5 g/dL, MCV 105 fL). WCC and platelets are normal. Blood film shows macrocytosis with dysplastic neutrophils. Bone marrow: hypercellular with dysplastic erythroid precursors. Diagnosis: MDS with isolated anaemia.
- Case 2 — Pancytopenia with Infections: A 70-year-old woman presents with recurrent chest infections and bruising. FBC: Hb 8.9 g/dL, WCC 2.5 ×10⁹/L, platelets 70 ×10⁹/L. Film shows hypogranular neutrophils and anisopoikilocytosis. Bone marrow: trilineage dysplasia. Diagnosis: MDS presenting with pancytopenia.
- Case 3 — Macrocytic Anaemia Misdiagnosed as B12 Deficiency: A 68-year-old man with fatigue is treated for “B12 deficiency” but fails to improve despite supplementation. Hb 9.0 g/dL, MCV 108 fL, normal B12/folate. Film: dysplastic neutrophils with pseudo–Pelger-Huët anomaly. Diagnosis: MDS mimicking megaloblastic anaemia.
- Case 4 — Transformation Risk: A 65-year-old woman with known low-risk MDS is followed in clinic. Over 18 months, her blast count increases from 3% to 18%. She develops worsening anaemia and thrombocytopenia. Diagnosis: High-risk MDS with progression towards acute myeloid leukaemia (AML).
- Case 5 — Secondary (Therapy-Related) MDS: A 60-year-old man treated with chemotherapy and radiotherapy for Hodgkin lymphoma 7 years ago presents with fatigue and bruising. FBC: Hb 8.7 g/dL, WCC 3.0 ×10⁹/L, platelets 55 ×10⁹/L. Bone marrow: dysplasia with cytogenetic abnormalities (del(5q), monosomy 7). Diagnosis: Therapy-related MDS.
Teaching Commentary 🧬
Myelodysplastic syndromes are clonal bone marrow disorders causing ineffective haematopoiesis and risk of transformation to AML. They typically affect older adults. Clinical features: anaemia, infections, bruising/bleeding. Labs: macrocytosis, cytopenias, dysplastic neutrophils (e.g. pseudo–Pelger-Huët cells), and abnormal marrow morphology. Risk stratification is via IPSS-R score (cytogenetics, blasts, cytopenias). Management ranges from supportive (transfusions, erythropoietin) to disease-modifying (azacitidine, lenalidomide in 5q-), and allogeneic stem cell transplant in selected younger patients. Always suspect therapy-related MDS in patients with prior chemo/radiotherapy.