| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
OSCE Breast Anatomy Exam
Related Subjects: |OSCE Eye Exam |OSCE Ear Exam |OSCE Abdominal Exam |OSCE Ascites Exam |OSCE Jaundice Exam |OSCE Testicular Exam |OSCE Inguinal Exam |OSCE Upper limb Neurology |OSCE Lower limb Neurology |OSCE Face Neurology |OSCE Breast exam
👩⚕️ Overview of Breast Examination
The breast examination is a critical clinical skill to identify abnormalities in breast tissue. It combines inspection and palpation, aiming to detect benign or malignant changes early. The breast consists of glandular, connective, and adipose tissues, with the primary role of milk production.
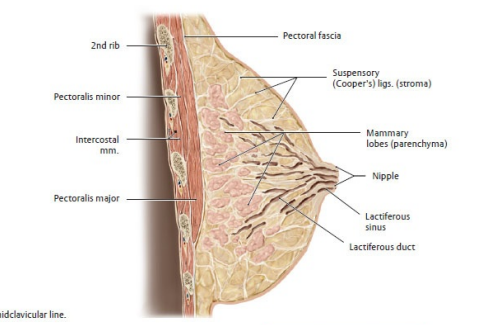
🔎 1. Anatomy Recap
- Nipple 👉 central milk outlet.
- Areola 👉 pigmented zone with sebaceous (Montgomery’s) glands.
- Lobules 🧬 milk-producing glands.
- Ducts 🧵 carry milk to nipple.
- Adipose tissue 🧈 bulk & shape.
- Fibrous connective tissue 🪢 suspensory (Cooper’s) ligaments.
- Blood supply 💉 internal mammary & lateral thoracic arteries.
- Lymphatics 🧩 axillary, supraclavicular, internal mammary nodes.
🛠️ Preparation
- Ensure privacy, offer a chaperone, and gain consent ✅.
- Explain procedure clearly and check patient comfort.
- Position: sitting upright for inspection, supine with pillow under shoulder for palpation.
- Expose to the waist while preserving dignity with drapes.
👀 Inspection
- Compare both breasts for size, shape, symmetry, contour.
- Skin changes 🟤: dimpling, puckering, redness, rash, peau d’orange.
- Nipple 👁️: inversion, retraction, discharge, ulceration.
- Dynamic manoeuvres:
- Arms raised overhead 🙆♀️ (hidden retraction becomes visible).
- Hands pressed on hips 💪 (contract pectoralis to reveal tethering).
- Leaning forward ➡️ look for asymmetry & contour change.
✋ Palpation
- Patient supine, ipsilateral arm raised behind head.
- Use pads of fingers, not tips, with systematic approach:
- 📏 Vertical strip pattern (best sensitivity).
- 🌀 Spiral pattern.
- 🔻 Wedge pattern (radial).
- Palpate all quadrants + tail of Spence (axillary extension).
- Comment on any lump: site, size, shape, surface, consistency, mobility, relation to skin/chest wall.
- Palpate nipple/areola for discharge or subareolar masses.
🧩 Lymph Node Examination
- Axillary nodes (central, anterior, posterior, lateral, apical).
- Supraclavicular & infraclavicular nodes.
- Cervical chain if suspicious spread.
📋 Common Findings
- Normal ✅: symmetrical, smooth tissue, no lumps, no skin/nipple changes, no lymphadenopathy.
- Benign 🌸:
- Fibroadenoma – smooth, mobile, “breast mouse”.
- Cyst – smooth, fluctuant, may be tender premenstrually.
- Suspicious/Malignant ⚠️:
- Hard, irregular, tethered lump.
- Skin changes: dimpling, peau d’orange, ulceration.
- Nipple retraction, bloody discharge.
- Axillary lymphadenopathy.
📝 Documentation
- Record lumps: site (clock-face position), size (cm), consistency, mobility, surface, tenderness.
- Skin & nipple changes.
- Lymph node status.
- Patient’s own reported symptoms.
🎓 Patient Education
- Encourage monthly self-breast awareness (not rigid “exams” but familiarity with normal baseline).
- Discuss NHS breast screening programme (mammography every 3 years from age 50–70).
- Explain red-flag symptoms 🚩: persistent lump, nipple discharge (esp. bloody), new inversion, skin tethering.
✅ Summary
The breast exam requires a calm, respectful approach: Inspection → Palpation → Node assessment. Document carefully, reassure the patient, and escalate if suspicious findings are present. Patient education on self-awareness and screening plays a key role in early cancer detection.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
