| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Postural Orthostatic Tachycardia Syndrome (POTS)
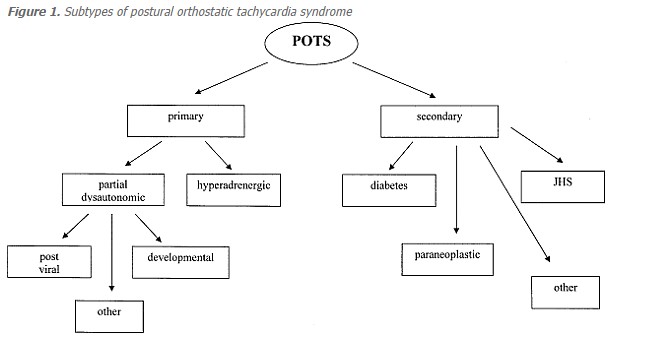
🩺 Postural orthostatic tachycardia syndrome (POTS) is the final common pathway of a heterogeneous group of underlying disorders that share similar clinical features.
📖 About
- POTS is not a single disease but a syndrome – a collection of disorders leading to the same clinical picture.
- 🧠 Autonomic dysfunction is central to its pathophysiology.
🧬 Aetiology (Unclear cause)
- ⚖️ Neuroendocrine dysfunction
- 🦠 Small fibre neuropathy
- 🌡️ Mast cell activation
- ⬆️ High plasma norepinephrine levels
📏 Definition: Diagnostic Criteria
- ❤️ Heart rate increase ≥ +30 bpm on standing (within 10 min)
- 🧍 Symptoms worsen with standing, improve with lying down
- ⏳ Symptoms persist > 6 months
- 🚫 No other overt cause of orthostatic tachycardia (e.g. bleeding, dehydration, meds)
🩺 Clinical Features
- 👩 Female:Male ratio ≈ 5:1
- 🦠 Often triggered by viral illness, COVID, pregnancy, immunisation, sepsis, surgery, or trauma
- 💓 Orthostatic intolerance with palpitations, fatigue
- 😵 Frequent lightheadedness, presyncope
- 🏃 Exercise intolerance, dyspnoea on exertion
- 📉 Symptoms worse around menstruation
- 🛌 Fatigue, poor sleep, daytime somnolence
- 🌐 IBS, joint hypermobility, abnormal sweating
- 🦵 ~50% show dependent acrocyanosis (red-blue discolouration of legs, cold to touch)
🦵 Dependent Acrocyanosis
🔎 Investigations
- 🧪 Bloods: FBC, U&E, LFTs, CRP → typically normal
- 📈 ECG: usually normal at rest
- 🫀 Echo: normal
- 📊 24h Holter: episodic tachycardia
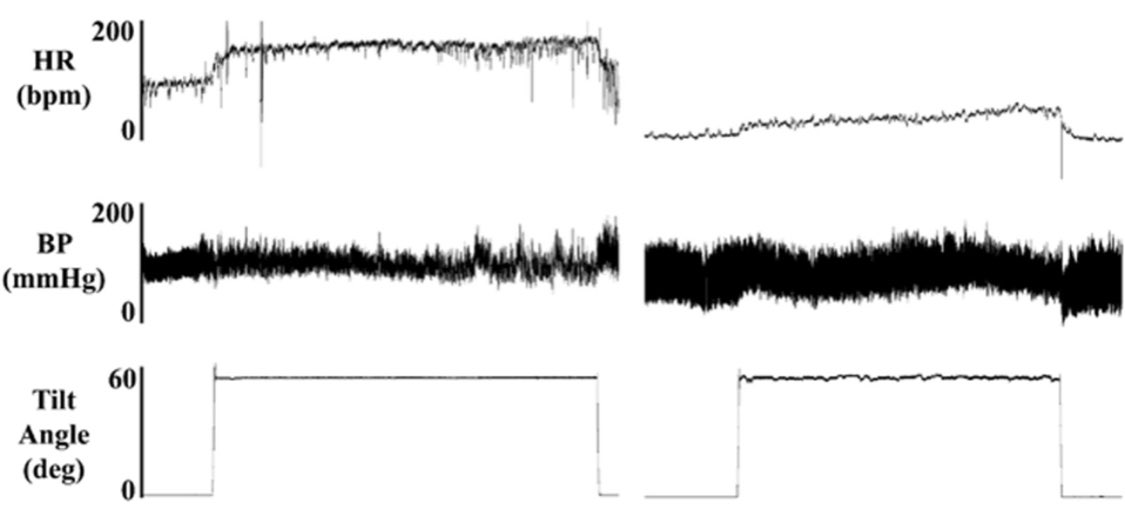
- 🪜 Tilt-table test: diagnostic, reproduces HR rise and symptoms
💊 Management
- 🚫 Stop contributing drugs: antidepressants, antihypertensives, alcohol, opiates, sildenafil
- 🏃♀️ Reconditioning: gradual aerobic exercise (20 min, 3×/week)
- 💧 IV saline (1L over 1–2h) for short-term/emergency benefit
- 🧦 Compression stockings (30–40 mmHg)
- 🥤 Hydration: 2 L/day
- 🧂 Salt loading: +2–4 g/day (monitor for oedema)
- 💊 Fludrocortisone 0.1–0.2 mg OD (risk: hypoK, hypoMg, oedema)
- 💊 Desmopressin (occasional use; risk: hyponatraemia)
- 💊 Midodrine 5–10 mg TDS (risk: nausea, scalp pruritus, supine HTN)
- 💊 Beta-blockers (metoprolol) in adolescents
- 💉 Erythropoietin in severe refractory cases (↑ blood volume & vascular tone)
- ✨ Management is trial and error – goal is symptom relief and quality of life.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
