Amiodarone
⚠️ Important: Side effects of Amiodarone can be severe. Long-term treatment is specialist-initiated only, reserved for life-threatening arrhythmias or where no safer alternative exists.
🫀 Amiodarone is a highly effective antiarrhythmic (Class III) but is irritant — extravasation can cause serious tissue injury.
Patients must be fully counselled before long-term use.
📖 About
- 💊 Very effective antiarrhythmic with multi-class actions.
- 🩺 Long-term therapy only started by a cardiologist.
- ⚡ Originally an antianginal; later repurposed as antiarrhythmic.
- 🧂 Structurally related to thyroxine and contains iodine → thyroid effects common.
🧠 Mode of Action
- Primarily a K⁺ channel blocker (Class III) → prolongs action potential and refractory period.
- Also blocks Na⁺ (Class I) and Ca²⁺ (Class IV) channels.
- Exhibits alpha- & beta-blocking effects (Class II-like).
- Slows His–Purkinje conduction and accessory pathways (e.g., WPW).
- Has vagolytic + vasodilatory effects.
⚗️ Pharmacokinetics
- Highly lipophilic, accumulates in fat, liver, and muscle.
- Metabolised in the liver → active metabolite desethylamiodarone.
- 📅 Very long half-life: 20–100 days (longer in elderly) → delayed toxicity & interactions.
🩺 Indications
- 🚑 Emergency use: VF/pulseless VT (after 3rd shock).
- 💓 Ventricular arrhythmias (VT, VF).
- ⚡ Atrial fibrillation/flutter (esp. with structural heart disease or WPW).
- Wide-complex tachycardias of uncertain origin.
🚫 Contraindications
- Pre-existing thyroid disease (contains iodine).
- Marked sinus bradycardia or advanced AV block (unless paced).
- Severe hypotension, iodine hypersensitivity.
⚠️ Major Side Effects
- 🫀 Bradycardia, AV block, QT prolongation → risk of Torsades (rare vs other Class III).
- 🫁 Pulmonary toxicity: interstitial pneumonitis, fibrosis (potentially fatal).
- 🧂 Thyroid dysfunction: hypo- or hyperthyroidism.
- 🧠 Tremor, ataxia, peripheral neuropathy.
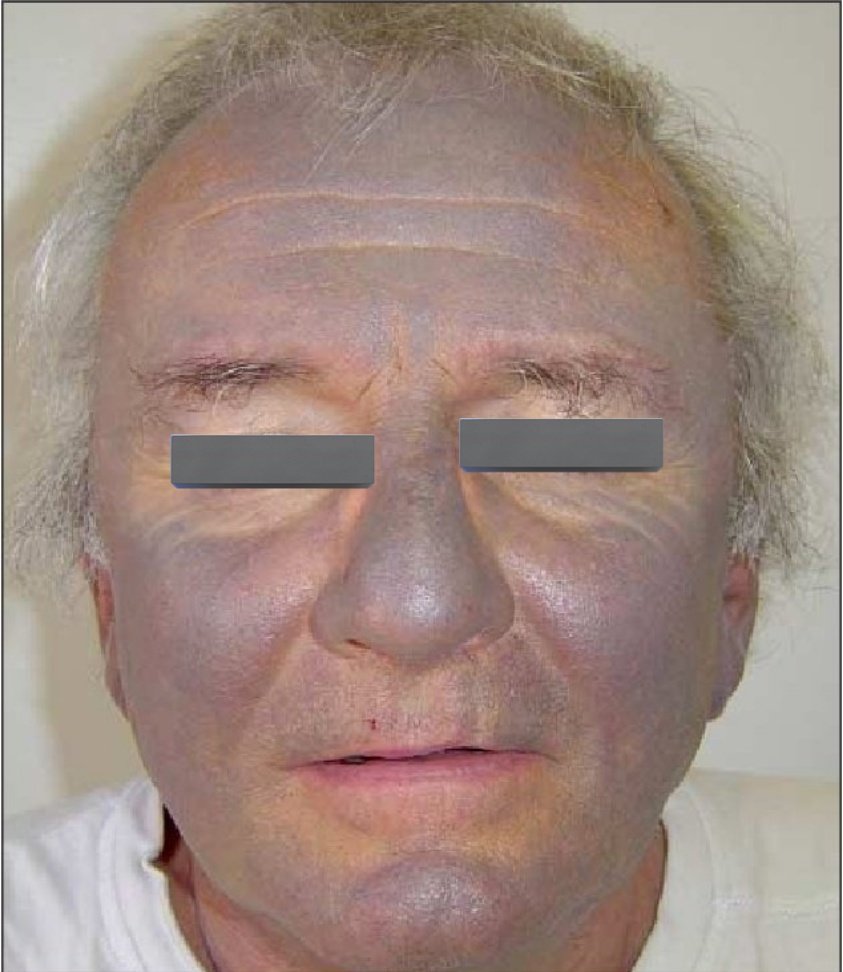
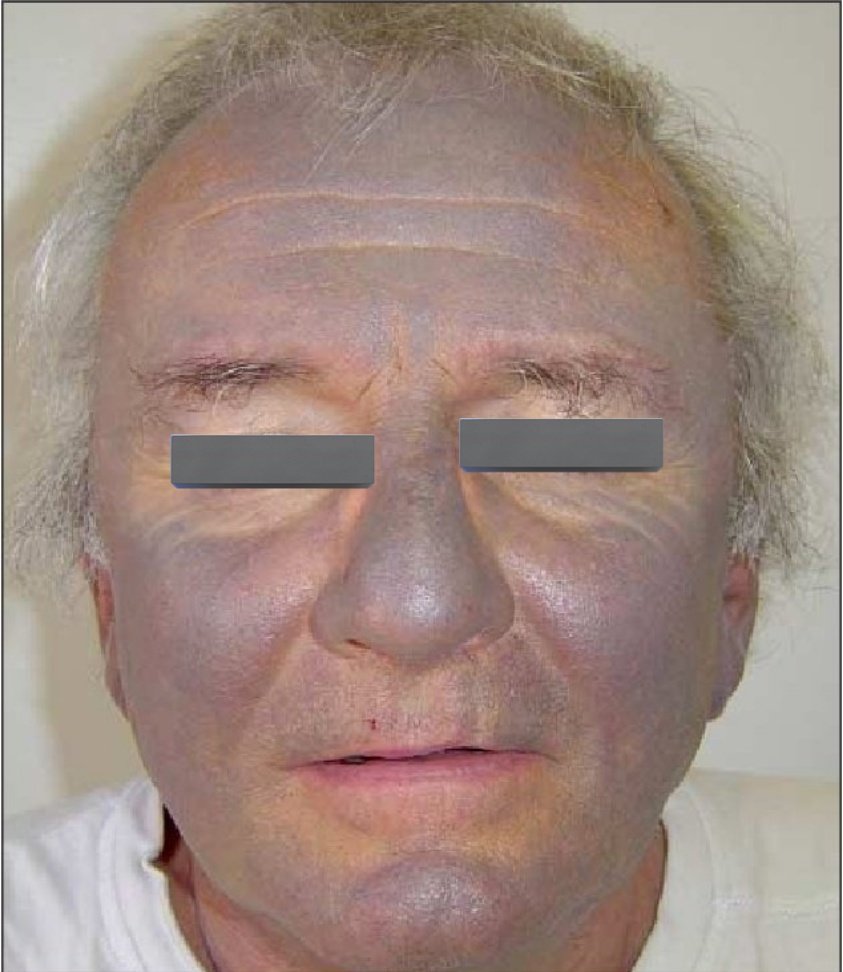
- 🩻 Slate-grey skin pigmentation, photosensitivity, rash.
- 👁️ Corneal microdeposits (reversible, halos around lights).
- 🫀 Rare: retroperitoneal fibrosis, orchitis, hepatitis.
- ⚡ IV use: hypotension & phlebitis if infused peripherally too fast.
🔗 Interactions
- ↑ INR with Warfarin (monitor closely).
- ↑ Digoxin and Phenytoin levels (reduce doses accordingly).
- Multiple CYP450 interactions → always check BNF.
💉 Dose Range (check BNF)
| Indication |
Dose |
Route |
| 🚑 Cardiac Arrest (VF/pulseless VT) |
300 mg IV in 20–30 ml NS/D5W (after 3rd shock) |
IV bolus |
| ⚡ Acute Arrhythmia |
150–300 mg IV over 30–60 min → then 900 mg/24h |
IV infusion (central line preferred) |
| 📅 Oral Loading |
200 mg TDS × 1 wk → 200 mg BD × 1 wk → 200 mg OD |
PO |
🩺 Monitoring
- Baseline & 6-monthly: TFTs, LFTs, U&E.
- Annual: CXR (pulmonary toxicity).
- Ophthalmology review if visual symptoms.
- Advise on sun protection (photosensitivity risk).
📚 References