| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Methanol Toxicity
Related Subjects: |Drug Toxicity - clinical assessment |Metabolic acidosis |Aspirin or Salicylates toxicity |Ethylene glycol toxicity |Ethanol toxicity |Methanol toxicity |Ricin toxicity |Carbon Tetrachloride Toxicity |Renal Tubular Acidosis |Lactic acidosis |Iron Toxicity |Tricyclic Antidepressant Toxicity |Opiate Toxicity |Carbon monoxide Toxicity |Benzodiazepine Toxicity |Paracetamol (Acetaminophen) toxicity |Amphetamine toxicity |Beta Blocker toxicity |Calcium channel blockers toxicity |Cannabis toxicity |Cyanide toxicity |Digoxin Toxicity |Lithium Toxicity |NSAIDS Toxicity |Ecstasy toxicity |Paraquat toxicity |Quinine toxicity |SSRI Toxicity |Theophylline Toxicity |Organophosphate (OP) Toxicity |Toxin elimination by dialysis |Drug Toxicity with Specific Antidotes
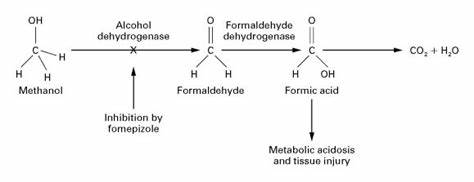
🧪 Alcohol dehydrogenase inhibition is the cornerstone of methanol toxicity treatment. Antidotal therapy — with fomepizole or, if unavailable, ethanol — must be initiated immediately to prevent conversion of methanol into its toxic metabolites, formaldehyde and formic acid. Delay in antidote administration is the single biggest predictor of blindness and death.
📖 About
- Methanol poisoning is a classic example of a treatable toxic metabolic acidosis — it presents with a high anion and osmolar gap and characteristic visual and CNS toxicity.
- Outbreaks occur after ingestion of illicit alcohol (“moonshine”) or adulterated spirits, or through exposure to industrial solvents (e.g., antifreeze, cleaning fluid).
- Even a few millilitres can be lethal: as little as 10 mL may cause blindness; 30 mL can be fatal.
🧬 Aetiology & Pathophysiology
- Methanol itself is relatively inert until metabolised by hepatic enzymes.
- Step 1: Methanol → (via Alcohol Dehydrogenase, ADH) → Formaldehyde.
- Step 2: Formaldehyde → (via Aldehyde Dehydrogenase) → Formic Acid.
- Formic acid is a mitochondrial toxin that inhibits cytochrome oxidase → impaired oxidative phosphorylation → severe lactic acidosis.
- It accumulates particularly in optic nerves and basal ganglia → visual loss and neurological injury.
- Half-life of formic acid ≈ 20 hours (longer in metabolic acidosis or renal failure).
🔍 Common Sources
- Windscreen washer fluid, antifreeze, solvents, model engine fuel.
- Illicit spirits or industrial alcohol substitutes.
- Laboratory methanol or contaminated ethanol-based products.
🧠 Clinical Presentation
- 🕐 Latent phase (6–24h): patient may appear intoxicated or mildly unwell.
- 🧍 Systemic: Headache, dizziness, nausea, vomiting, abdominal pain.
- 🫁 Respiratory: Deep, rapid “Kussmaul” breathing due to metabolic acidosis.
- 👁️ Ophthalmic: Blurred vision, photophobia, “snow field” vision, progressing to blindness (optic neuritis).
- 🧠 Neurological: Confusion, agitation, seizures, coma.
- 🧪 Late: Severe acidosis, renal failure, visual loss, or respiratory arrest.
🧾 Investigations
- Blood tests: FBC, U&E (look for AKI), LFT, calcium (↓), CK if rhabdomyolysis suspected.
- ABG: Metabolic acidosis with raised anion gap (≥16 mmol/L).
- Osmolar gap: Elevated (>10–15 mOsm/kg) — early diagnostic clue before acidosis develops.
- Lactate: Falsely elevated due to formate interference in analyzers.
- Methanol level: Confirmatory but rarely available quickly — do not delay antidote.
- Urinalysis: May show calcium oxalate crystals (if mixed ethylene glycol ingestion).
- Imaging: CT/MRI: bilateral basal ganglia necrosis (putaminal lesions) in delayed cases.
📉 Key Diagnostic Triad
- 1️⃣ High anion gap metabolic acidosis
- 2️⃣ Raised osmolar gap
- 3️⃣ Visual or neurological symptoms
⚕️ Management Overview
Immediate priorities: Resuscitate → Antidote → Correct acidosis → Dialyse → Supplement folate
🏥 1. Immediate Stabilisation
- Secure airway, breathing, and circulation (ABCs).
- Administer oxygen (target SpO₂ 94–98%).
- IV fluids to maintain perfusion and enhance renal clearance.
- Monitor glucose — hypoglycaemia is common.
- Insert urinary catheter if oliguric; assess fluid output.
🧪 2. Antidotal Therapy
- Goal: Inhibit alcohol dehydrogenase to stop toxic metabolite formation.
- Fomepizole (preferred):
- Loading: 15 mg/kg IV over 30 min.
- Maintenance: 10 mg/kg every 12 h × 4 doses, then 15 mg/kg every 12 h until methanol <20 mg/dL, pH normalised, and asymptomatic.
- During haemodialysis: give same dose every 4 h (it is dialysable).
- Ethanol (if fomepizole unavailable):
- 5% solution: 15 mL/kg loading, then 2 mL/kg/h maintenance.
- 10% solution: 7.5 mL/kg loading, then 1 mL/kg/h maintenance.
- 40% spirits (emergency oral): 2 mL/kg loading, then 0.25 mL/kg/h.
- Double infusion rate for chronic alcohol users (enzyme induction).
- Therapeutic blood ethanol level: 100 mg/dL (22 mmol/L).
🧫 3. Correct Metabolic Acidosis
- Administer IV sodium bicarbonate if pH <7.25 or HCO₃⁻ <15 mmol/L.
- Monitor venous pH, K⁺, and lactate.
- Target pH >7.3 to improve formate metabolism.
🧬 4. Enhance Elimination
- Haemodialysis: Rapidly removes methanol, formate, and corrects acidosis.
- Indications:
- pH <7.25 or HCO₃⁻ <10
- Visual symptoms or coma
- Serum methanol >50 mg/dL (15 mmol/L)
- Renal failure or rising creatinine
- Continue until methanol undetectable and acidosis resolves.
🌿 5. Cofactor Therapy
- Folinic acid (Leucovorin): 50 mg IV/PO every 4–6 h for 24–48 h. → Accelerates formate metabolism to CO₂ and water.
- If folinic acid unavailable: give Folic acid 50 mg IV or 10 × 5 mg tablets orally.
- Thiamine (100 mg IV) and pyridoxine (50 mg IV) are added if ethylene glycol ingestion possible.
⚠️ 6. Monitoring
- Repeat ABG, osmolar gap, and electrolytes every 2–4 hours.
- Monitor vision daily — irreversible damage may occur within 24 h.
- Maintain careful fluid balance; watch for pulmonary oedema if large fluid loads given.
🧩 Treatment Summary Table
| Parameter | Treatment Approach | Notes |
|---|---|---|
| pH >7.2, HCO₃⁻ >20 | Observation ± oral ethanol | Mild poisoning; observe ≥24 h |
| pH 7.0–7.2, HCO₃⁻ 10–20 | Bicarbonate + ethanol/fomepizole ± dialysis | Moderate toxicity |
| pH <7.0 or HCO₃⁻ <10 | Bicarbonate + fomepizole + dialysis + folate | Severe, life-threatening |
🚫 Contraindications
- No absolute contraindication to antidote therapy — delay is more harmful.
- Relative: known allergy to fomepizole (use ethanol instead).
💊 Common Side Effects of Antidotes
- Ethanol: Hypoglycaemia, CNS depression, hypotension.
- Fomepizole: Headache, mild rash, transient ↑ liver enzymes, injection-site irritation.
📚 References
- Methanol Intoxication: Diagnostic and Treatment Approach. Am J Kidney Dis 2016.
- Methanol Poisoning Information (Methanol Institute)
- TOXBASE: Methanol and Ethylene Glycol Management Guidelines
- Brent J. “Fomepizole for Toxic Alcohol Poisoning.” N Engl J Med 2009;360:2216–2223.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
