| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Absence Seizure
⚡ Key point: Absence seizures are brief (5–20 seconds), start and end abruptly, and the child typically resumes activity as if nothing happened. Because they can occur many times per day, they may quietly but significantly disrupt learning and quality of life.
💡 Terminology & Classification
- The older term “petit mal epilepsy” is now obsolete and should be avoided.
- Absence seizures belong to the generalised seizure group.
- ILAE (2017) recognises three useful clinical categories:
- Typical absences – abrupt onset and offset of impaired awareness, lasting seconds; EEG shows classic 3 Hz generalised spike-and-wave. Seen in childhood absence epilepsy (CAE) and juvenile absence epilepsy (JAE).
- Atypical absences – slower onset/offset, often longer, with less clear loss of awareness; EEG shows < 2.5 Hz spike-and-wave; usually in epileptic encephalopathies (e.g. Lennox–Gastaut).
- Absences with special features – absences accompanied by eyelid myoclonia (Jeavons), myoclonus, or prominent automatisms.
- When documenting, try to state the absence type and, where possible, the epilepsy syndrome (e.g. CAE, JAE, Lennox–Gastaut).
📌 About
- Part of the generalised non-motor (absence) seizure spectrum.
- Typical childhood absences: onset usually between ages 4–8, more common in girls 👧 than boys 👦.
- Children are often otherwise neurologically normal; persistent uncontrolled absences can impair concentration and school progress.
🧬 Aetiology
- Often presumed genetic, reflecting abnormal thalamo–cortical network excitability.
- Family history of generalised epilepsy is common but not universal.
🩺 Clinical Features
- 📉 May present with an unexplained decline in school performance or “daydreaming” reported by teachers/parents.
- 👁️ Brief lapses in consciousness: blank stare, unresponsive, often with subtle eyelid flutter or blinking.
- 👄 Small automatisms (lip smacking, fumbling) or mild facial/myoclonic jerks may occur.
- ⏱️ Duration: typically < 10–20 seconds with no post-ictal confusion.
- 🔁 Frequency: can occur dozens to hundreds of times per day.
- 🌬️ Often provoked by hyperventilation (useful clinically and during EEG testing).
🔎 Investigations
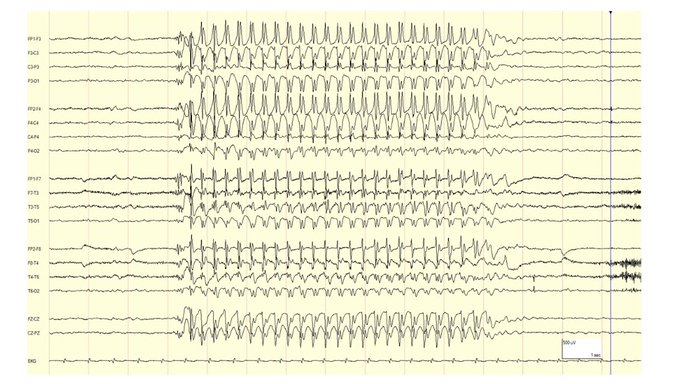
- 🧾 EEG: Generalised, symmetric 3 Hz spike-and-wave discharges in typical absences (classically activated by hyperventilation). Between seizures the EEG may be normal or show brief spike–wave bursts.
- 🧲 MRI brain: Usually normal in typical CAE/JAE. Perform imaging if there are atypical features (focal signs, developmental delay, abnormal neurology, atypical EEG pattern).
- 🧪 Metabolic / other tests: Reserved for atypical cases or when developmental, metabolic or syndromic causes are suspected.
🧠 EEG Example
💊 Management
- In pure childhood absence epilepsy, seizures often remit in adolescence (many by ~12 years), though a minority later develop generalised tonic–clonic seizures.
- ⚠️ Safety advice: avoid swimming unsupervised, climbing heights, or cycling on busy roads until seizures are well controlled.
- First-line for typical absence with no other seizure types: Ethosuximide – generally well tolerated; rare but important adverse effects include blood dyscrasias, skin reactions, and hepatic or renal impairment (monitor FBC and LFTs as per local guidance).
- Alternatives:
- Valproate – effective for typical absence, myoclonic and tonic–clonic seizures, but in the UK has major restrictions in females of childbearing potential because of teratogenicity and neurodevelopmental risks, as well as hepatotoxicity and pancreatitis.
- Lamotrigine – useful when ethosuximide/valproate are unsuitable (e.g. in girls/young women), but can occasionally worsen myoclonus and carries a risk of serious skin reactions (including Stevens–Johnson syndrome).
- Treatment choice should balance seizure control, adverse-effect profile, and (for girls) future pregnancy and contraception; UK practice follows MHRA and NICE guidance.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
