| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
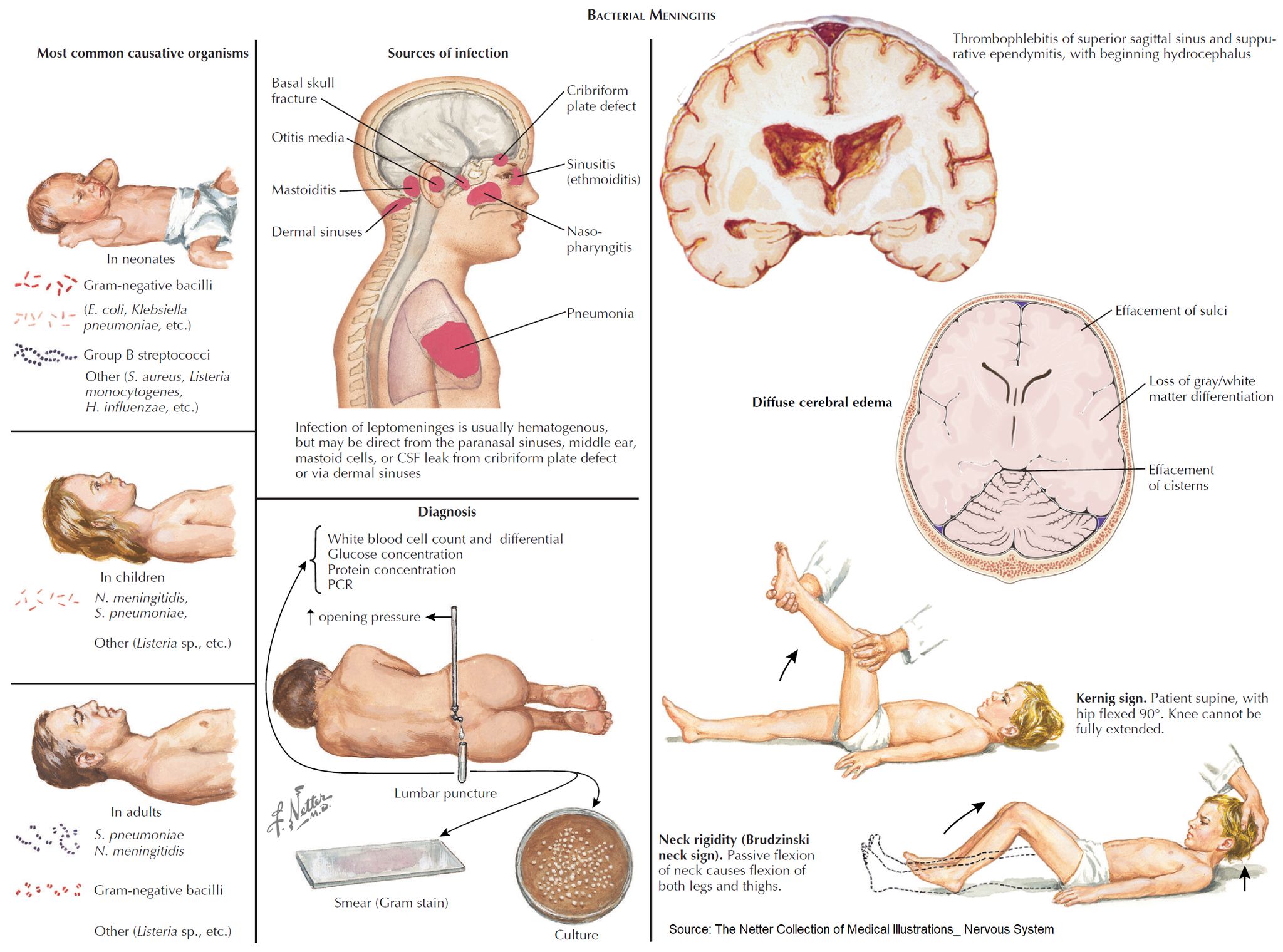
Neonatal meningitis
Related Subjects: |Lumbar Puncture |CSF Interpretation |CSF Rhinorrhoea
👶🧠 Neonatal meningitis – Definitive diagnosis is made by CSF examination via lumbar puncture (LP). LP should be performed in any neonate suspected of sepsis/meningitis, but ⚠️ treatment must not be delayed while awaiting results.
📖 About
- Occurs within the first 90 days of life 🍼.
- Most often bacterial, and is a life-threatening emergency 🚨.
🩺 Clinical Presentation
- ⚠️ Classical triad (fever, stiff neck, vomiting) often absent.
- Instead look for:
- ❌ Poor feeding, irritability, lethargy
- 😴 Apnoea, listlessness, reduced tone
- 🌡️ Fever OR hypothermia
- ⚡ Seizures
- 🚩 Other red flags: bulging fontanelle, high-pitched cry, hypoglycaemia, metabolic acidosis, shock, pallor
🦠 Microbiology
- Group B Streptococcus (GBS) 🧬 → ~50% (esp. type III; vertical transmission).
- Escherichia coli (K1 capsule) 🦠 → ~20%.
- Listeria monocytogenes 🥗 → 5–10% (contaminated food in pregnancy).
- Viruses 🦠 → HSV, VZV (less common, but important for prognosis).
⚠️ Complications
- ♿ Cerebral palsy (~8%)
- 📘 Learning disability (~7%)
- ⚡ Persistent seizures (~7%)
- 👂 Hearing loss (~25%)
- 🧠 Hydrocephalus, abscess, or subdural effusion
👶➡️👧 Causes in Older Infants (>3 months)
- Streptococcus pneumoniae 🧬
- Neisseria meningitidis 💉
- Haemophilus influenzae type b (Hib) 💊 (much less common since vaccination).
💊 Management
- 🚑 Immediate IV antibiotics (before LP if unstable):
- Ampicillin + Cefotaxime (UK NICE guidance) 💉
- Avoid ceftriaxone in neonates (risk of kernicterus) ❌
- 💧 Supportive care: fluids, oxygen, seizure control (phenobarbital/levetiracetam).
- 🦠 If HSV suspected: add Acyclovir 🧪
- 🔊 Hearing test follow-up (due to high risk of deafness).
- 🧪 Close monitoring: blood cultures, CSF studies, CRP trends.
- 👩👦 Public health: maternal screening & prophylaxis for GBS at delivery reduces risk.
🧑🏫 Exam Tip
Neonatal meningitis is one of the few conditions where the common organisms differ significantly from older children. Always think GBS, E. coli, and Listeria 👶 — whereas after 3 months, pneumococcus and meningococcus dominate.
Cases — Neonatal Meningitis
- Case 1 — Early-onset GBS infection 🍼: A 3-day-old term infant presents with poor feeding, irritability, and fever. Exam: bulging fontanelle, lethargy. CSF: neutrophilia, low glucose, high protein. Blood culture: Group B Streptococcus. Diagnosis: early-onset neonatal meningitis (GBS). Managed with IV benzylpenicillin + gentamicin, then tailored antibiotics.
- Case 2 — E. coli meningitis 🦠: A 10-day-old preterm baby develops temperature instability, seizures, and poor tone. Mother had prolonged rupture of membranes. CSF: Gram-negative bacilli, low glucose, high protein. Culture: E. coli K1. Diagnosis: neonatal meningitis due to E. coli. Managed with IV cefotaxime for 21 days.
- Case 3 — Listeria infection 🥛: A 14-day-old infant presents with poor feeding, apnoea, and irritability. Mother ate unpasteurised cheese during pregnancy. CSF: mononuclear predominance, positive Gram-positive bacilli. Diagnosis: Listeria monocytogenes meningitis. Managed with IV ampicillin + gentamicin.
Teaching Point 🩺: Neonatal meningitis is most often caused by Group B Strep, E. coli, or Listeria. - Early onset (<7 days): GBS, E. coli, Listeria (maternal transmission). - Late onset (>7 days): same organisms + nosocomial Gram-negatives. Presents non-specifically (poor feeding, irritability, temperature instability, seizures). Management: urgent IV antibiotics + supportive care. Mortality and neurological sequelae remain high.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
