| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Tropheryma whipplei (Whipple disease)
🌍 In 1907, George Hoyt Whipple first described Whipple’s disease in a missionary with chronic diarrhoea, arthritis, fever, and weight loss. It remained uniformly fatal until the 1960s, when antibiotics transformed the prognosis. Whipple later received the Nobel Prize (1934) for work on anaemia, though not directly for this disease. Today, Whipple’s disease is a rare but treatable multisystem infection caused by Tropheryma whipplei.
📖 About
- Chronic systemic infection due to Tropheryma whipplei, a Gram-positive actinomycete.
- Classically affects middle-aged Caucasian men (M:F ratio ~10:1).
- Manifests as malabsorption with multisystem involvement.
- Fatal without treatment, but now curable with long-term antibiotics.
🧬 Aetiology & Pathogenesis
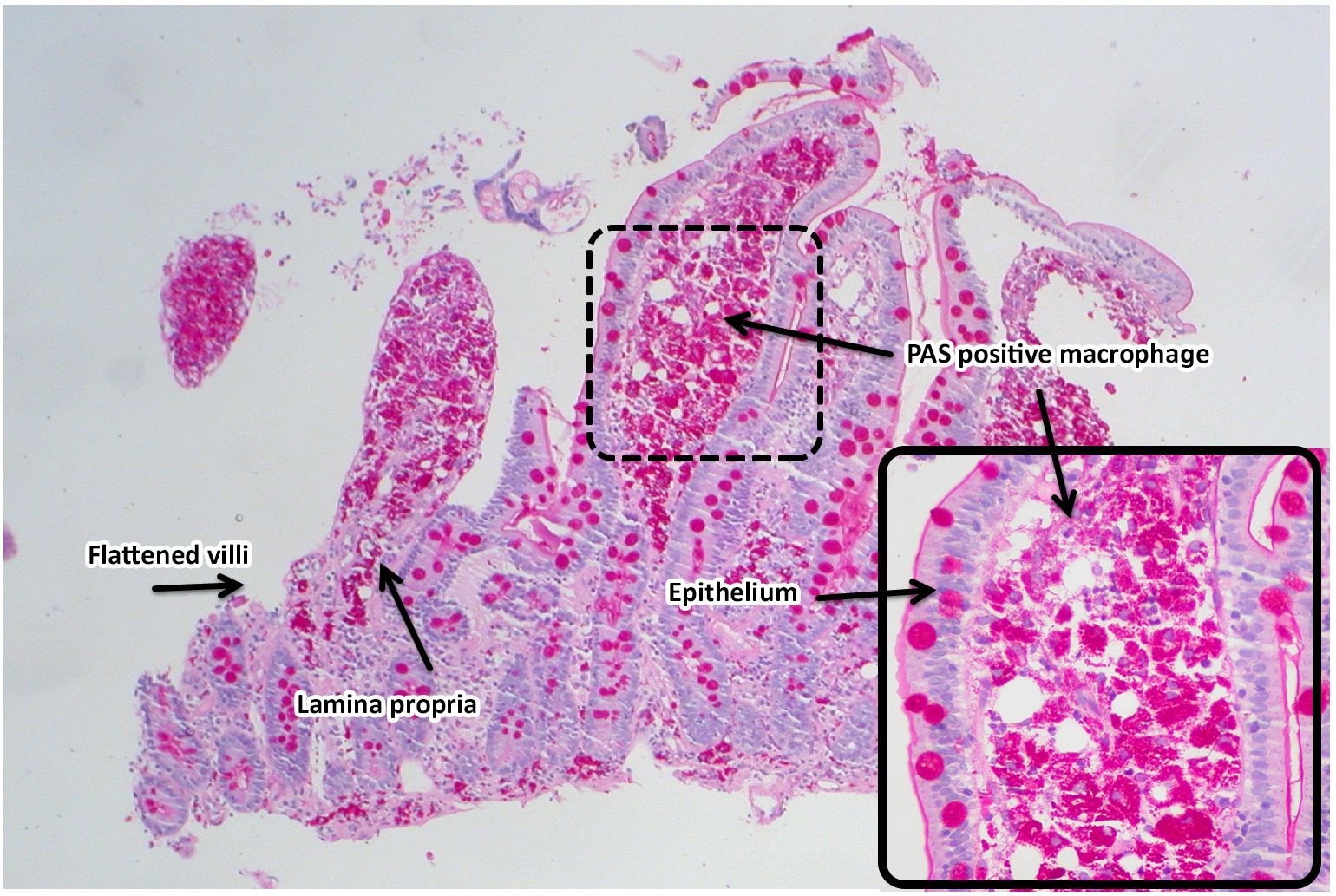
- Macrophages loaded with PAS-positive material (but acid-fast negative).
- Thought to represent a host defect in intracellular bacterial killing rather than exposure alone.
- Possible genetic predisposition — increased frequency of HLA-B27 and impaired Th1 response.
- Organism ubiquitous in the environment, but disease remains rare.
🔎 Key Characteristics
- Gram-positive bacillus; culture is very difficult (only possible in specialised labs).
- Detected by PCR of stool, saliva, or biopsy samples in research settings.
- Histology hallmark: foamy macrophages packed with PAS-positive granules in the lamina propria.
🩺 Clinical Features
- GI: Malabsorption → chronic diarrhoea, steatorrhoea, weight loss, abdominal pain, bloating.
- MSK: Migratory arthritis or arthralgia often precedes GI symptoms by years.
- Cardiac: Pericarditis, endocarditis (culture-negative), arrhythmias.
- Respiratory: Pleurisy, chronic cough.
- Neuro: Dementia, ophthalmoplegia, facial myoclonus, hypothalamic syndrome (polydipsia, hyperphagia, sleep disturbance).
- Other: Lymphadenopathy, skin pigmentation, clubbing, uveitis, papilloedema.
 🧪 Investigations
🧪 Investigations
- Bloods: Normocytic or microcytic anaemia, lymphopenia, ↑ESR, ↓albumin, ↓cholesterol, ↓carotene.
- Electrolyte imbalance: hypokalaemia, hypocalcaemia, hypomagnesaemia.
- Jejunal biopsy: diagnostic — foamy PAS-positive macrophages infiltrating lamina propria.
- CSF involvement possible — check if neurological features.
- PCR for T. whipplei (stool, saliva, or tissue) increasingly used but not universally available.
🧾 Differentials
- Coeliac disease (similar malabsorption picture).
- GI tuberculosis or atypical mycobacterial infection (e.g. MAI).
- Histoplasmosis (fungal infection with PAS-positive macrophages).
- Small bowel lymphoma, amyloidosis.
- NSAID-induced enteropathy.
💊 Management
- Initial therapy: IV ceftriaxone 2 g daily or IV penicillin G for 2–4 weeks.
- Maintenance: Oral trimethoprim–sulfamethoxazole (960 mg BD) for 12 months.
- Alternatives: doxycycline + hydroxychloroquine; co-amoxiclav also used.
- Relapse is common if treatment incomplete — lifelong monitoring required.
- Correct malnutrition and replace electrolytes (K, Mg, Ca, vitamins).
- Reversible cause of dementia → early recognition is crucial.
📊 Prognosis
- Dramatically improved with antibiotics; 5-year survival excellent if treated early.
- Neurological involvement carries poorer prognosis and risk of relapse.
- Relapse can occur even years after treatment → long-term follow-up needed.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
