| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Hyponatraemia
Related Subjects: | Sodium Physiology | Hyponatraemia | TURP Hyponatraemia syndrome | Hypernatraemia | Diabetes Insipidus
⚠️ Hyponatraemia: A sudden drop in serum sodium (Na⁺) can cause cerebral oedema → cellular swelling, seizures, and coma. 🧠 Severe cases risk brain herniation. ⏳ Chronic/gradual decline is better tolerated. 📈 Correction must be <12 mmol/L per day (ideally 6–8 mmol/L/24h) to avoid Central Pontine Myelinolysis (CPM).
| 🚨 Comatose Management (Severe Hyponatraemia Na <115 mmol/L) |
|---|
|
🧬 Physiology
- Low Na⁺ → suppresses ADH release (normally increases water excretion).
- SIADH → inappropriate ADH secretion → water retention, ↑ urine osmolality.
- Hypovolaemia → ADH & thirst ↑, aldosterone promotes Na reabsorption.
- Result = water shifts intracellularly → cerebral oedema.
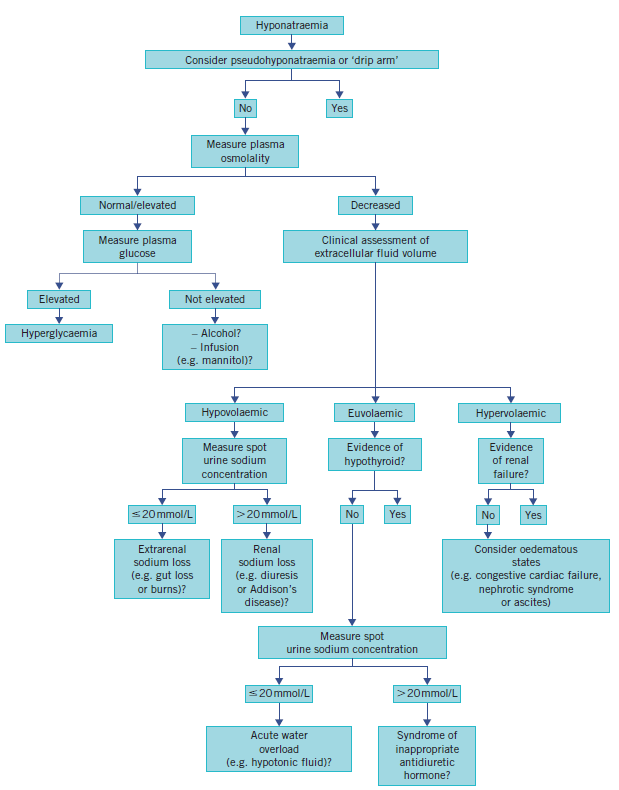
📊 Clinical Evaluation
- Check drug history, fluid balance, exam hydration status.
- Hypovolaemic: Dehydrated, dry mucous membranes, hypotension. (Causes: GI losses, Addison’s, burns, diuretics).
- Euvolaemic: Normal exam, SIADH common. (Causes: SSRIs, NSAIDs, post-op, pain, stress, psychogenic polydipsia).
- Hypervolaemic: Oedema, ascites, HF, CKD, cirrhosis, iatrogenic fluids, post-TURP syndrome.
🧾 Causes of Hyponatraemia
- Hypovolaemic: GI losses, diuretics, Addison’s, salt-wasting nephropathy.
- Euvolaemic: SIADH, drugs, pain, stress, post-TURP, psychogenic polydipsia.
- Hypervolaemic: HF, CKD, cirrhosis, iatrogenic fluids.
- Pseudohyponatraemia: Hyperlipidaemia or hyperproteinaemia → lab artefact.
📉 Severity & Symptoms
- 🔺 Rapid fall or Na <120 mmol/L → symptomatic risk ↑.
- Na 110–115 → headache, confusion, irritability.
- Na <110 → seizures, coma, ataxia (medical emergency).
🔬 Investigations
- 🧪 U&E: Mild (135–130), Moderate (125–129), Severe (<125).
- 🧪 Serum Osmolality: <275 in true hypoNa.
- 🧪 Urine Osmolality: >100 in SIADH.
- 🧪 Urine Na: <20 in hypovolaemia, >30 in SIADH.
- 🔎 TFTs & Cortisol (exclude hypothyroid/adrenal insufficiency).
- 📷 CXR (lung cancer, pneumonia → SIADH).
- 🧠 CT Head (exclude bleed, tumour, infection).
⚠️ Central Pontine Myelinolysis (CPM)
🧠 Risk of overly rapid correction of chronic hypoNa → demyelination (esp. pons). ➡️ Irreversible deficits: dysarthria, quadriplegia, locked-in syndrome. ⛔ Keep correction ≤12 mmol/L/day.
📈 Algorithm
🩺 Management Principles
- ✅ ABC first. Admit severe cases to HDU/ITU.
- 🔄 Frequent Na checks (2–4h), strict fluid balance.
- 💉 Hypovolaemia: IV normal saline → reassess.
- 🚰 SIADH/Euvolaemia: Fluid restrict (800–1000 ml/day). In seizures/coma → 3% saline bolus (~5 mmol/L correction).
- 💊 Persistent SIADH: Tolvaptan or Demeclocycline.
- 🧾 Addison’s: Short Synacthen Test → IV hydrocortisone.
- 🌊 Hypervolaemic: Restrict salt & water, loop diuretics if needed.
📚 References
- Diagnosis & Management of Inpatient Hyponatraemia and SIADH
- Guidelines for Hyponatraemia Management (RLBUHT)
🩺 Case 1 — Hypovolaemic Hyponatraemia
A 72-year-old woman presents with vomiting and diarrhoea for 4 days. She is confused, BP 90/60 mmHg, pulse 110 bpm, mucous membranes dry. Labs: Na⁺ 124 mmol/L, urea and creatinine raised. Management: 💧 IV 0.9% saline cautiously to restore volume, monitor sodium rise. Identify and treat cause (e.g. gastroenteritis). Avoid: ❌ Rapid correction (>8–10 mmol/L per 24 h) as this risks osmotic demyelination syndrome (ODS).
🩺 Case 2 — Euvolaemic Hyponatraemia (SIADH)
A 68-year-old man with a history of small-cell lung cancer presents with confusion and seizures. He is euvolaemic on exam. Labs: Na⁺ 116 mmol/L, low plasma osmolality, inappropriately concentrated urine. Management: 🚰 Fluid restriction, consider demeclocycline or vasopressin receptor antagonists in refractory cases; treat underlying cause (e.g. lung cancer). Hypertonic saline in severe symptomatic cases under specialist care. Avoid: ❌ Isotonic saline — may worsen hyponatraemia in SIADH. Avoid rapid correction.
🩺 Case 3 — Hypervolaemic Hyponatraemia
An 80-year-old man with decompensated heart failure presents with breathlessness, ankle swelling, and Na⁺ 128 mmol/L. Exam shows raised JVP, pitting oedema, bibasal crackles. Management: 💊 Fluid and salt restriction, loop diuretics, optimise heart failure therapy (ACEI/ARNI, beta-blocker, MRA). Avoid: ❌ Rapid overcorrection; avoid excessive IV fluids which worsen overload.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
