| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Malaria Falciparum (Includes Cerebral Malaria)
Related Subjects: |Fever in a traveller |Malaria Falciparum |Malaria Non Falciparum |Viral Haemorrhagic Fevers (VHF) |Lassa fever |Dengue |Marburg virus disease |AIDS HIV |Yellow fever |Ebola Virus |Leptospirosis |Crimean-Congo haemorrhagic fever |African Trypanosomiasis (Sleeping sickness) |American Trypanosomiasis (Chagas Disease) |Incubation Periods |Notifiable Diseases UK
⚠️ Always consider falciparum malaria in anyone with a flu-like illness returning from an endemic area within the last 3 months. 👉 Send urgent thick and thin films, inform the lab, and involve Infectious Diseases early. ⏱ A patient can deteriorate and die before the post-take ward round – the diagnosis must be suspected at first contact.
| 🚑 Initial Management – Complicated Disease |
|---|
|
📖 About
- Falciparum malaria is the most lethal form – death may occur within hours.
- Any red cell involvement >2% = severe disease.
- BNF Malaria Guidance
🦟 Vector & Parasite
- Spread by the female Anopheles mosquito.
- Caused by the protozoan parasite Plasmodium falciparum.
- Other routes: transfusion, needlestick, “airport malaria” (imported mosquitoes).
 🧬 Pathophysiology
🧬 Pathophysiology
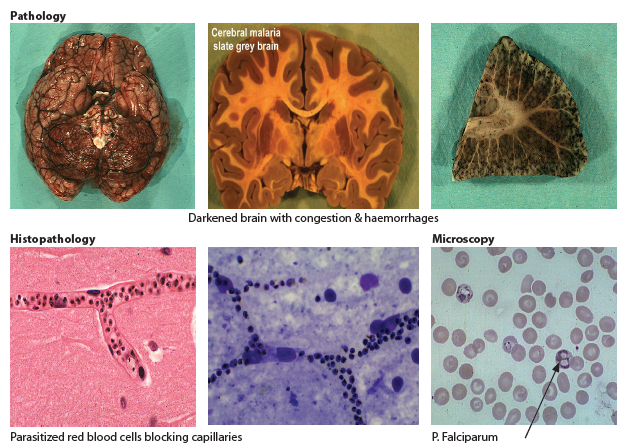
- Cytoadherence: Infected RBCs stick to endothelium → block venules.
- Mediated by PfEMP-1 on red cell surface.
- Leads to cerebral, renal, pulmonary, and multi-organ damage.
- Rosetting: Infected cells clump with normal RBCs, worsening occlusion.
🌍 Epidemiology
- ~1 million deaths per year globally.
- Endemic in Sub-Saharan Africa, SE Asia, and parts of South America.
- In the UK, malaria is an imported disease.
🔄 Life Cycle (Simplified)
- 🦟 Mosquito bite → sporozoites enter liver.
- 🩸 Liver stage → merozoites released into blood.
- RBC stage → multiplication and rupture of RBCs (rigors, fever, anaemia).
- Adherence to endothelium → organ damage (brain, kidney, lung, gut).
- Flu-like illness: fever, malaise, headache, rigors.
- Hepatosplenomegaly (mild).
- Severe: cerebral malaria → coma, seizures, hemiparesis, blindness.
⚠️ Complications
- Coma, seizures (reduced GCS).
- Acute renal failure (10% need dialysis).
- Metabolic acidosis, hypoglycaemia (from parasite + quinine).
- Severe anaemia, haemolysis, jaundice.
- “Blackwater fever” (haemoglobinuria).
- DIC, thrombocytopenia.
- ARDS / non-cardiogenic pulmonary oedema.
🧪 Investigations
- Bloods: FBC, U&E, LFTs, glucose, lactate, blood cultures.
- Films: 3–5 thick & thin blood films over 48 hrs. Thick = parasite detection, Thin = speciation + parasitaemia %.
- Parasitaemia >5% or pre-schizont forms → poor prognosis.
- Rapid antigen detection (useful in UK hospitals).
- Other: CXR (pneumonia), urinalysis, stool culture, COVID test if relevant.
🔎 Differentials (coinfection possible!)
- Dengue, Typhoid, Schistosomiasis, Tick typhus.
- TB, Dysentery, Influenza, Viral or bacterial pneumonia.
- HIV, bacterial sepsis, meningitis.
💊 Management (BNF-linked)
- 🟢 Uncomplicated falciparum malaria (oral):
- Quinine 5–7 days + doxycycline (7 days) or clindamycin (7 days).
- Atovaquone-proguanil (Malarone).
- Artemether-lumefantrine (Riamet).
- 🔴 Complicated malaria:
- Resuscitate: ABCDE, HDU/ICU, fluids + glucose monitoring.
- IV Artesunate (preferred) 2.4 mg/kg at 0, 12, 24 hrs then daily.
- Alternative: IV Quinine 20 mg/kg loading → 10 mg/kg 8-hourly. Switch to oral once stable. Complete 7-day course with doxycycline/clindamycin.
- Correct hypoglycaemia, treat bacterial co-infection, manage seizures.
- 🤰 Pregnancy:
- Extremely high risk (esp. 3rd trimester).
- Quinine is safe; add clindamycin (not doxycycline).
- Specialist input: Artesunate may be used in severe cases.
📞 UK Expert Advice
- PHE Malaria Reference Laboratory: 020 7637 0248
- NaTHNaC: 0845 602 6712
- HPS Travax (Scotland): www.travax.nhs.uk
- Regional Centres: Birmingham, Liverpool, London, Oxford
Cases — Malaria (Plasmodium falciparum)
- Case 1 — Uncomplicated Malaria in a Traveller: A 27-year-old man returns from Nigeria with fever, chills, sweats, and headache 10 days after travel. He did not take prophylaxis. Exam: febrile, mild jaundice, splenomegaly. Blood film: parasitaemia 2% with ring forms. Diagnosis: Uncomplicated falciparum malaria. Management: Oral artemisinin-based combination therapy (artemether-lumefantrine) if able to tolerate orally; admit for monitoring.
- Case 2 — Severe Malaria with Cerebral Involvement: A 34-year-old woman presents after returning from India with confusion, seizures, and fever. Exam: GCS 9, splenomegaly. Bloods: Hb 7.5 g/dL, lactate raised, parasitaemia 8%. Diagnosis: Severe falciparum malaria with cerebral involvement. Management: Admit to ICU. IV artesunate (first-line) or IV quinine if unavailable, supportive care for seizures and hypoglycaemia, careful fluid balance.
- Case 3 — Malaria in Pregnancy: A 22-year-old woman at 26 weeks’ gestation, recently returned from Ghana, presents with fever, myalgia, and vomiting. Exam: febrile, tachycardic, mild hepatosplenomegaly. Blood film confirms falciparum malaria, parasitaemia 4%. Diagnosis: Falciparum malaria in pregnancy. Management: IV artesunate if severe; if uncomplicated and able to tolerate oral therapy: artemisinin-based combination therapy (artemether-lumefantrine) or quinine + clindamycin (depending on gestation and national guidelines). Urgent obstetric + infectious disease review.
Teaching Commentary 🦟
*P. falciparum* is the most dangerous malaria species due to its ability to cause high parasitaemia, microvascular sequestration, and multi-organ dysfunction. - Uncomplicated malaria: fever, sweats, headache, splenomegaly — treat with oral ACT. - Severe malaria: cerebral features, acidosis, renal failure, shock, high parasitaemia — treat with IV artesunate. - Pregnancy: higher risk of severe disease, miscarriage, and low birth weight. Key principles: confirm diagnosis with thick and thin blood films (or rapid antigen tests), admit all falciparum malaria cases initially, and escalate to ICU if severe.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
