| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
CT Basics for Stroke
Related Subjects: |Acute Stroke Assessment (ROSIER&NIHSS) |Atrial Fibrillation |Atrial Myxoma |Causes of Stroke |Ischaemic Stroke |Cancer and Stroke |Cardioembolic stroke |CT Basics for Stroke |Endocarditis and Stroke |Haemorrhagic Stroke |Stroke Thrombolysis |Hyperacute Stroke Care
🧠 Introduction
- 💡 Stroke medicine evolved rapidly with the introduction of CT scanning, enabling clinicians to distinguish between ischaemic and haemorrhagic strokes quickly and safely. Non-contrast CT (NCCT) is the initial investigation of choice for nearly all suspected strokes.
- ⚙️ CT imaging is central to acute stroke management — it determines stroke type, rules out mimics, and guides emergency therapies such as thrombolysis or thrombectomy.
- 📜 Before CT, differentiating stroke subtypes relied on clinical signs or even post-mortem findings. Early diagnostic methods (e.g. pineal calcification displacement) were crude and unreliable.
📚 History of CT Imaging
- 🧑🔬 Sir Godfrey Hounsfield developed the first CT scanner in 1972 — funded by EMI’s Beatles record profits 🎸.
- 🧩 The first clinical CT scan in 1971 (Atkinson Morley Hospital, London) diagnosed a cerebral cyst — a landmark moment in neuroradiology.
- 🏥 By the late 1980s, CT became routine in major hospitals, revolutionising stroke diagnosis and management.
⚙️ Technical Aspects of CT
- 🌀 A CT scanner uses a rotating X-ray tube and detectors to capture cross-sectional images of the body, reconstructed by a computer into slices.
- 🔁 Helical (spiral) CT introduced in the 1990s enabled continuous scanning for 3D reconstructions — essential for vascular imaging.
- 📏 Image density is expressed in Hounsfield Units (HU):
- Air = -1000 HU
- Water = 0 HU
- Grey matter ≈ +35 HU
- Acute haemorrhage ≈ +70 HU
- Bone = +400 to +3000 HU
☢️ Radiation Exposure
- CT involves ionising radiation and is regulated under IRMER in the UK — only to be performed when clinically justified.
- 🧮 A typical CT head ≈ 2 mSv → roughly equivalent to 100 chest X-rays.
- 🌍 Natural background radiation ≈ 3.1 mSv/year for comparison.
| Scan Type | Approx. Radiation Dose (mSv) |
|---|---|
| 🌍 Natural Background | 3.1 / year |
| 🧠 Brain CT | 2.0 |
| 🫁 Chest CT | 7.0 |
| 🫀 Chest + Abdomen + Pelvis | 21.0 |
🏥 CT in Acute Stroke
- CT is first-line for suspected stroke — rules out haemorrhage before thrombolysis or thrombectomy.
- Indications: sudden focal neurological deficit, decreased consciousness, headache, or anticoagulant use.
- ⚠️ Early CT may appear normal within first 6 hours of ischaemia — correlate with clinical findings.
🔍 CT Interpretation Tips
🧩 Review CT systematically from vertex to base. Look for hyperdensities (clots), hypodensities (oedema or infarction), and mass effect. Always exclude mimics such as subdural haematoma or tumour before giving thrombolysis.
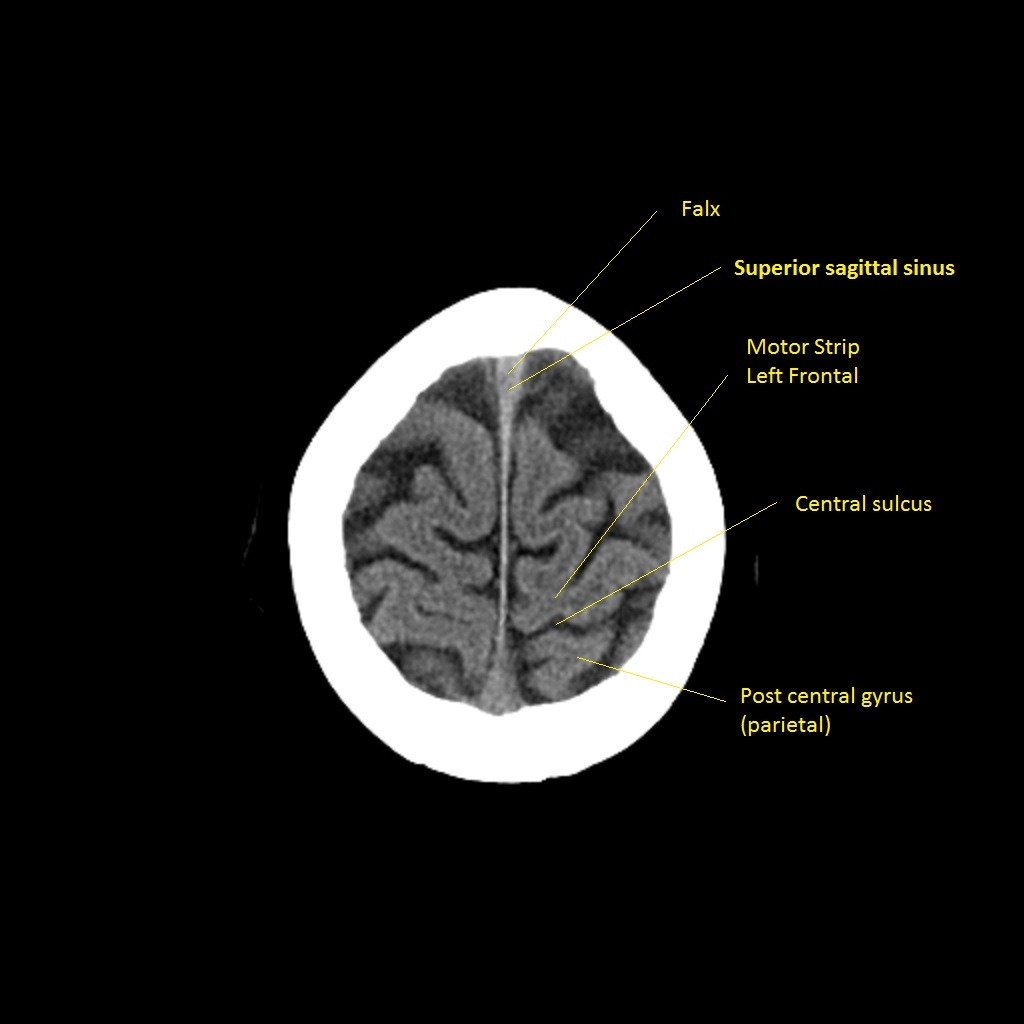
🧠 Early Signs of Ischaemia on CT
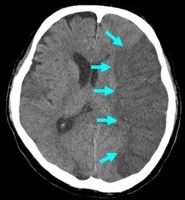
- ⚡ Hyperdense MCA sign: Thrombus in middle cerebral artery — earliest visible clue.
- 🌫️ Loss of grey-white differentiation: Early cytotoxic oedema, especially in cortex or basal ganglia.
- 🌀 Insular ribbon sign: Blurring between insular cortex and adjacent white matter.
- 🌊 Effacement of sulci: Local swelling and oedema flattening cortical grooves.
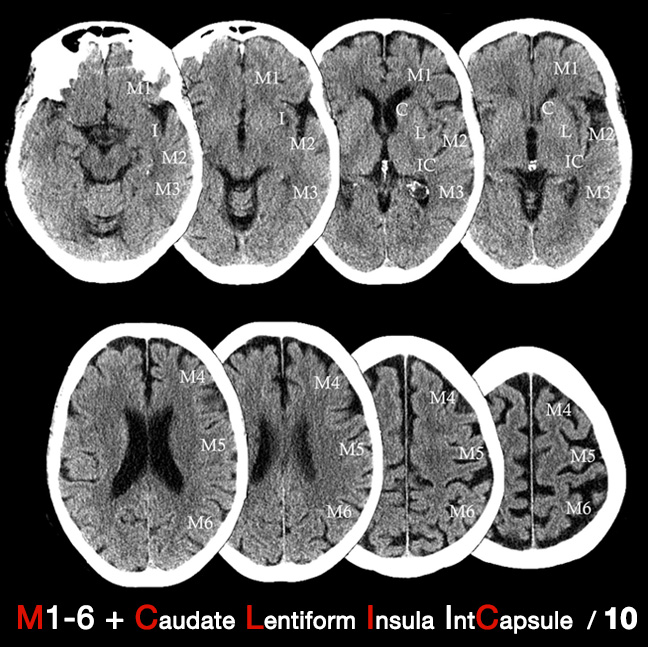
🧮 ASPECTS Score
The Alberta Stroke Program Early CT Score (ASPECTS) assesses early ischaemic change in MCA territory. • Score = 10 (normal), decreasing with extent of infarction. • ASPECTS ≤ 7 → poorer prognosis & higher risk of post-thrombolysis haemorrhage.
🩸 CTA & CT Perfusion (CTP)
- 🧩 CT Angiography (CTA): Maps arteries from aortic arch → Circle of Willis; identifies clots, dissections, or stenosis. Essential before thrombectomy.
- 🎯 CT Perfusion (CTP): Measures blood flow (CBF), volume (CBV), and mean transit time (MTT). Differentiates core infarct vs. penumbra (salvageable tissue).
⚠️ Limitations of CT
- ❌ May miss small brainstem strokes or subtle early cortical ischaemia.
- 🧩 False negatives possible in first few hours; false positives from leukoaraiosis in elderly.
🕓 Later CT Signs (6–24 hours)
- ⬜ Hypodense areas become obvious due to cytotoxic and vasogenic oedema.
- 💔 Haemorrhagic transformation may occur, especially in large infarcts or with anticoagulant use.

💡 Teaching tip: - NCCT remains the first-line scan for stroke — fast, reliable, and accessible. - Subtle early changes demand a trained eye and careful side-by-side comparison. - Combine imaging findings with clinical localisation for accurate decision-making.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
