| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Polyarteritis nodosa (PAN)
Related Subjects: |Relapsing Polychondritis |Reactive Arthritis |Raynaud's Phenomenon |Polymyositis |Polyarteritis nodosa |Osteoporosis |Osteogenesis Imperfecta |Osteopetrosis |Polyarteritis nodosa |Rheumatoid Arthritis |Systemic Sclerosis (Scleroderma) |Rheumatology Autoantibodies |Overlap Syndrome |Inclusion Body Myositis |Inflammatory Myopathies |Psoriatic Arthritis |Adult Onset Still's Disease |Alkaptonuria |Behcet's Syndrome
💡 If a systemic vasculitis case is presented with hypertension, renal impairment, and is associated with Hepatitis B, always consider Polyarteritis Nodosa (PAN).
🧾 About
- PAN is a systemic necrotising vasculitis affecting medium and small arteries, usually sparing capillaries and venules.
- Leads to vessel wall inflammation, fibrinoid necrosis, thrombosis, microaneurysms, and tissue infarction.
🧬 Aetiology
- Strongly associated with Hepatitis B virus (HBV) and sometimes cryoglobulinaemia.
- Pathology hallmark: fibrinoid necrosis of vessel walls with inflammatory cell infiltration.
⚠️ Clinical Features
- Constitutional: PUO, fatigue, weight loss, myalgia, arthralgia.
- Neurological: Mononeuritis multiplex (painful, asymmetric motor/sensory deficits due to nerve ischaemia).
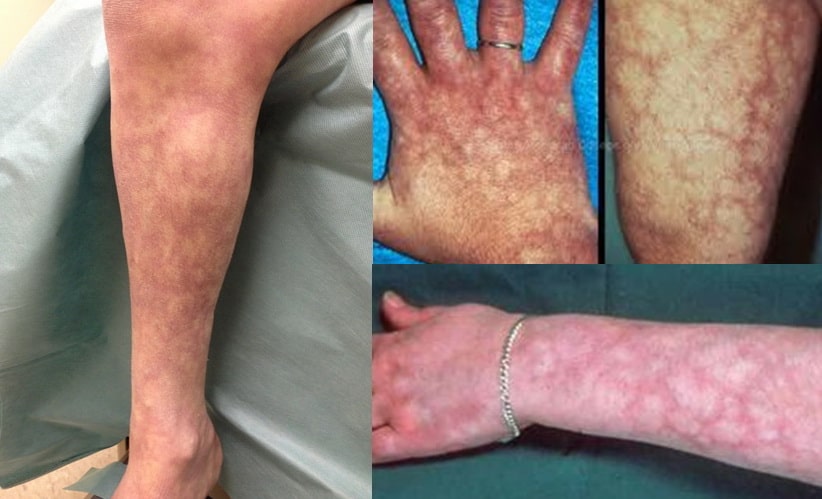
- Skin: Palpable purpura, livedo reticularis, subcutaneous nodules.
- Renal: Hypertension, renal impairment, haematuria, proteinuria without glomerulonephritis.
- Gastrointestinal: Abdominal pain (mesenteric ischaemia), risk of bowel infarction, orchitis in men.
- Cardiovascular: Myocardial infarction, pericarditis, and stroke risk increased.
🔬 Investigations
- Bloods: FBC (anaemia, raised WCC), ↑ ESR/CRP.
- Renal function: U&E for renal impairment.
- Hepatitis B serology: Key association.
- ANCA: Typically negative (helps distinguish from microscopic polyangiitis).
- Imaging: Angiography (renal/mesenteric) → “string of beads” microaneurysms.
- Biopsy: Fibrinoid necrosis + transmural inflammation of arteries.
💊 Management
- Multidisciplinary care: Nephrology, rheumatology, infectious diseases.
- Corticosteroids: High-dose steroids are mainstay.
- Immunosuppressants: Cyclophosphamide, azathioprine for severe disease.
- Antivirals: In HBV-associated PAN → antiviral therapy + possible plasma exchange.
Cases — Polyarteritis Nodosa (PAN)
- Case 1 — Systemic vasculitis 💉: A 45-year-old man presents with fever, weight loss, muscle aches, and abdominal pain. Exam: livedo reticularis over the thighs and tender nodules along medium-sized arteries. Labs: raised ESR/CRP, negative ANCA. Angiography: multiple microaneurysms of renal and mesenteric arteries. Diagnosis: classic systemic PAN. Managed with high-dose corticosteroids and cyclophosphamide.
- Case 2 — Renal involvement 🩸: A 52-year-old woman reports new-onset hypertension and haematuria. Exam: reduced renal function, BP 180/100 mmHg. Biopsy: necrotising arteritis of medium-sized renal arteries, no glomerulonephritis. Diagnosis: PAN with renal artery involvement. Managed with immunosuppression and blood pressure control.
- Case 3 — Hepatitis B–associated PAN 🦠: A 39-year-old man with chronic hepatitis B develops abdominal pain, mononeuritis multiplex (wrist and foot drop), and testicular pain. Angiography: aneurysms in mesenteric arteries. Diagnosis: HBV-associated PAN. Managed with antivirals, corticosteroids, and plasma exchange.
Teaching Point 🩺: Polyarteritis Nodosa is a necrotising vasculitis of medium-sized arteries. It classically spares the lungs, is ANCA-negative, and can cause systemic, renal, neurological, and gastrointestinal disease. Always check for hepatitis B association.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
