| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
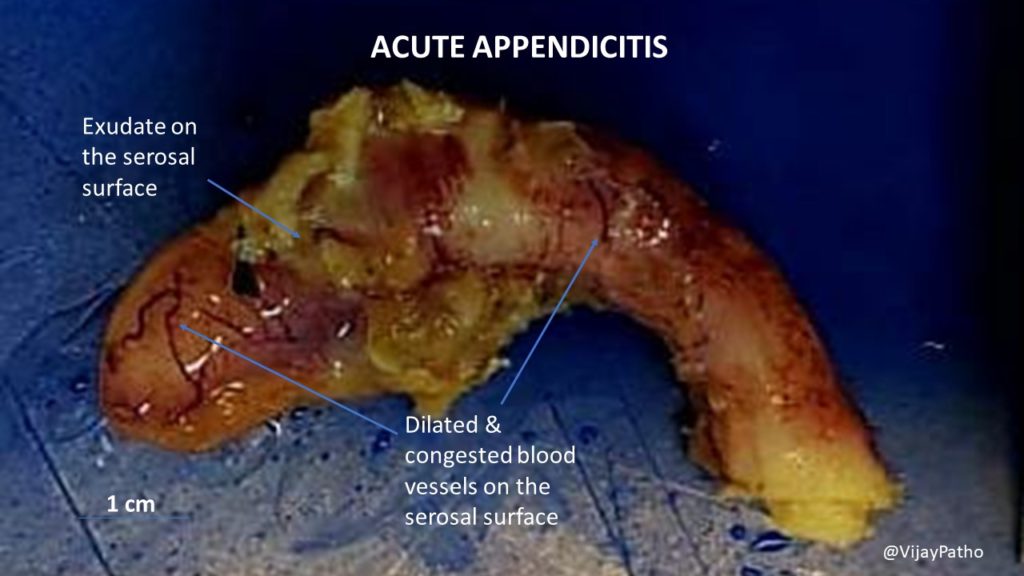
Acute Appendicitis
Related Subjects:Acute Cholecystitis |Acute Appendicitis |Acute Appendicitis in Children |Chronic Peritonitis |Acute Abdominal Pain/Peritonitis |Chronic Peritonitis |Abdominal Aortic Aneurysm |Ectopic Pregnancy |Acute Cholangitis |Acute Abdominal Pain/Peritonitis |Assessing Abdominal Pain |Penetrating Abdominal Trauma |Acute Pancreatitis |Acute Diverticulitis
Overview / Definition
Acute appendicitis is inflammation of the vermiform appendix, usually triggered by luminal obstruction and bacterial overgrowth. It is a common cause of acute abdominal pain requiring emergency surgical assessment, and untreated disease can progress to gangrene, perforation, peritonitis, sepsis, and abscess. Because symptoms overlap with gastroenteritis, urinary and gynaecological disease, diagnosis is fundamentally a clinical + trajectory problem supported by tests and imaging.
Epidemiology
- 📊 Lifetime risk: around 7–8%; incidence appears higher in men than women (e.g., ~8.6% vs ~6.7%).
- 👥 Age: peak in teens/early adulthood; extremes of age have higher perforation and atypical presentations.
- 🔍 Diagnostic reality: negative appendicectomy (normal histology) historically ~10–20%, reduced with modern imaging pathways.
Anatomy of the Appendix
- 📍 Blind-ended tube from caecum near the ileocaecal valve; variable length (often ~6–10 cm).
- 🧭 Positions: retrocaecal (~most common), pelvic, pre-/post-ileal, paracaecal—position changes symptoms.
- 🩸 Blood supply: appendicular artery (end-artery branch of ileocolic) → explains rapid ischaemia once pressure rises.
Pathophysiology
The core sequence is: obstruction → ongoing mucus secretion + closed loop → rising intraluminal pressure → venous congestion and lymphatic failure → bacterial proliferation → mural ischaemia → gangrene → perforation. Clinically this maps to a shift from vague visceral pain to sharp peritoneal pain as parietal peritoneum becomes involved. The most important teaching point for juniors: appendicitis is often a dynamic disease—a single exam can be misleading, so re-examination and escalation with deterioration are key.
Aetiology and Causes
- 🚧 Luminal obstruction: faecolith, lymphoid hyperplasia (esp. children), rarely tumour.
- 🦠 Infective triggers: viral illness → lymphoid hyperplasia; mixed gut flora contribute once obstruction occurs.
- 🐛 Parasites: e.g., Enterobius (pinworm) occasionally implicated/incidentally found.
Risk Factors
- 👶 Children and 👵 older adults: higher risk of delayed diagnosis and perforation.
- 💊 Immunosuppression/steroids: blunted inflammatory response (normal WCC/fever doesn’t reassure).
- 🤰 Pregnancy: atypical localisation and broader differential.
🩺 Clinical Features
- ➡️ Pain: classically peri-umbilical then migrates to RIF; worsens with movement/cough.
- 🤢 GI symptoms: anorexia and nausea common; vomiting typically follows pain (gastroenteritis often reverses this order).
- 🌡️ Systemic: low-grade fever and tachycardia; marked sepsis suggests perforation/abscess or alternative pathology.
- 💩 Bowel/urinary: diarrhoea/tenesmus (pelvic appendix), dysuria (adjacent bladder/ureter irritation).
Typical vs Atypical Presentations
- ✅ Typical: migration + RIF tenderness + anorexia + rising inflammatory markers.
- ⚠️ Atypical: retrocaecal (flank/back pain, minimal anterior guarding), pelvic (suprapubic pain, diarrhoea, urinary symptoms), elderly (subtle signs), pregnancy (pain may shift cephalad), immunosuppressed (few signs).
Pain Migration and Neuroanatomy
Early appendiceal inflammation irritates visceral afferents travelling with sympathetic fibres (often perceived peri-umbilically, roughly T10). As inflammation reaches the parietal peritoneum, somatic innervation produces localised, sharper RIF pain with guarding and rebound. This is a useful narrative to teach students: the exam finding (peritonism) is often a marker of disease stage and complication risk.
Examination Findings
- 👆 RIF tenderness (McBurney’s point), percussion/cough tenderness, guarding, rebound.
- ↪️ Rovsing’s sign (LLQ palpation causes RIF pain) supports peritoneal irritation.
- 🦵 Psoas sign (retrocaecal), obturator sign (pelvic).
- 🩺 Consider testicular exam in males (torsion mimic) and appropriate gynae assessment in females.
Special Populations
- 👶 Children: often labelled “gastroenteritis”; perforate earlier; use paediatric scores and ultrasound-first strategies.
- 👵 Elderly: less localised pain/fever; higher perforation and malignancy risk—image early if uncertain.
- 🤰 Pregnancy: localisation can shift; ultrasound first, MRI if equivocal; do not let a negative test override strong clinical concern.
- 💊 Immunocompromised: low threshold for imaging and senior review.
Differential Diagnosis
- 🦠 Gastroenteritis, mesenteric adenitis, constipation.
- 🧻 UTI/pyelonephritis, ureteric stone.
- 🩸 Gynae: ectopic pregnancy, ovarian torsion/cyst, PID.
- 🧠 IBD (Crohn’s terminal ileitis), Meckel’s diverticulitis, diverticulitis (esp. right-sided).
- 🔁 In older adults: caecal/appendiceal tumour (consider if atypical or complicated).
🔎 Investigations
Blood Tests
- 🩸 FBC (neutrophilia), CRP (may be normal early), U&E (dehydration/AKI), LFT, amylase/lipase as broader acute abdomen screen.
- 🧪 Lactate/VBG if sepsis or concern for ischaemia/perforation.
- 🧾 Group & save / crossmatch if significant sepsis or operative likelihood.
Urinalysis
- 💧 Useful to identify UTI; mild haematuria can occur from ureteric irritation and does not exclude appendicitis.
Pregnancy Testing
- 🤰 β-hCG in all females of reproductive potential—ectopic pregnancy is the dangerous mimic until proven otherwise.
Imaging
- 🖥️ CT A/P (adults): highly accurate; identifies alternative diagnoses and complicated disease features.
- 🩻 Ultrasound: first-line in children and pregnancy (graded compression); operator dependent.
- 🧲 MRI (pregnancy): recommended when ultrasound is non-diagnostic and suspicion persists.
Risk Stratification / Clinical Scoring
- 📐 Scores (e.g., Alvarado, AIR, paediatric scores) help organise thinking: low-risk patients may be observed; intermediate risk often imaged; high-risk needs early senior/surgical decision-making.
- ⚠️ Scores are adjuncts—never let a “low” score override clear peritonism or deterioration.
Initial Management
| ⚡ Initial Management |
|---|
|
Antibiotic Therapy
- 💊 Follow local antimicrobial guidance; aim for prompt therapy when complicated appendicitis is suspected.
- ✅ Simple/uncomplicated: peri-operative prophylaxis; many pathways advise no post-op antibiotics after source control.
- 💥 Complex/perforated/abscess/sepsis: IV broad-spectrum then step-down when improving; duration commonly guided by clinical response and source control (often ~3–7 days).
Example UK guidance: “simple = no post-op antibiotics; complex = minimum course with review/step-down
Surgical Management
- 🔪 Laparoscopic appendicectomy is standard for most patients: faster recovery, fewer wound infections, and allows inspection for alternative pathology.
- 🟠 Open appendicectomy may be chosen in selected cases (dense adhesions, technical factors, some complicated disease).
- 🕒 Timing: stable uncomplicated appendicitis is usually managed within an appropriate urgent window; unstable/septic/peritonitic patients need urgent senior review and source control planning.
Non-operative (Antibiotics-First) Management
- 🟡 Consider only in selected patients with imaging-confirmed uncomplicated appendicitis who can engage in shared decision-making and follow-up.
- 🔁 Key counselling: meaningful risk of recurrence or later appendicectomy; appendicolith increases failure/complication risk.
- 🚫 Not appropriate for peritonism, sepsis, perforation, abscess, or diagnostic uncertainty where a dangerous mimic remains possible.
Appendix Mass and Appendiceal Abscess
- 🧱 Presents after several days: tender RIF mass, persistent fever, raised CRP; CT often shows phlegmon ± collection.
- 🛡️ Typical approach: IV antibiotics, fluids, bowel rest; IR drainage if drainable abscess.
- 🔎 In older adults/atypical cases: arrange colonic assessment after recovery to exclude caecal malignancy.
⚠️ Complications
- 💥 Perforation → diffuse peritonitis and septic shock.
- 🛡️ Abscess / phlegmon; wound infection; intra-abdominal collections post-op.
- 🧵 Adhesions and later small bowel obstruction (rare but important).
- 🩸 VTE risk with acute inflammation/immobility.
Post-operative Care
- 🚶 Early mobilisation, analgesia plan, antiemetics; advance diet as tolerated.
- 🩺 Monitor for fever, rising pain, ileus, wound issues; low threshold for imaging if deteriorating (concern for collection).
- 🧪 Review histology (rare neoplasm can change follow-up).
- 🏠 Discharge: clear safety net (worsening pain, fever, vomiting, wound redness/discharge).
Outcomes and Prognosis
- ✅ Uncomplicated appendicitis treated promptly has excellent outcomes and short length of stay.
- ⏱️ Delayed diagnosis increases risk of perforation, abscess, prolonged antibiotics, and longer admission.
- 👶👵 Higher complication rates in children and older adults, largely driven by diagnostic delay and atypical features.
Common Pitfalls and Missed Diagnoses
- ⚠️ Over-reassurance by “normal” early CRP, especially if symptoms are <12 hours or patient is immunosuppressed.
- ⚠️ Anchoring on gastroenteritis when pain is focal/progressive or patient has peritoneal signs.
- ⚠️ In women: failing to exclude ectopic pregnancy/ovarian pathology.
- ⚠️ In older adults: not considering tumour-associated appendicitis or perforation with subtle exam.
Case-Based Examples
Case 1 (classic): 21-year-old with peri-umbilical pain migrating to RIF, anorexia, low-grade fever, guarding; WCC/CRP raised; CT confirms uncomplicated appendicitis → fluids, analgesia, peri-op antibiotics, laparoscopic appendicectomy.
Case 2 (pregnancy): 22 weeks gestation with RUQ/right flank pain and vomiting; ultrasound equivocal; MRI supports appendicitis → early surgical management with obstetric awareness.
Case 3 (mass/abscess): 55-year-old, 5 days symptoms, RIF mass; CT shows phlegmon + small collection → IV antibiotics ± drainage; plan follow-up colonic evaluation and selective interval surgery.
Key Learning Points / Exam Pearls
- 🧠 Appendicitis is trajectory-based: repeat exams and escalation with deterioration are critical.
- 🧭 Appendix position explains atypical symptoms (retrocaecal = flank/back; pelvic = urinary/diarrhoea).
- 🤰 Pregnancy: ultrasound first, MRI if equivocal; don’t let non-diagnostic imaging override strong clinical suspicion.
- 🩺 Analgesia early is good practice and does not invalidate the exam.
- 🟡 Antibiotics-first is for selected uncomplicated cases; perforation/sepsis/peritonism = surgical pathway.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
