| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Primary Open-Angle Glaucoma (POAG)
📖 Overview
- 🟢 POAG accounts for ~90% of all glaucoma cases.
- 😶 Silent disease: gradual, painless rise in intraocular pressure (IOP), often unnoticed until late.
- ⚠️ Typically asymptomatic until significant optic nerve damage and visual field loss occur → importance of early screening.
🧬 Aetiology
- 📈 Progressive rise in IOP (often 20–30 mmHg) damages the optic nerve head over years.
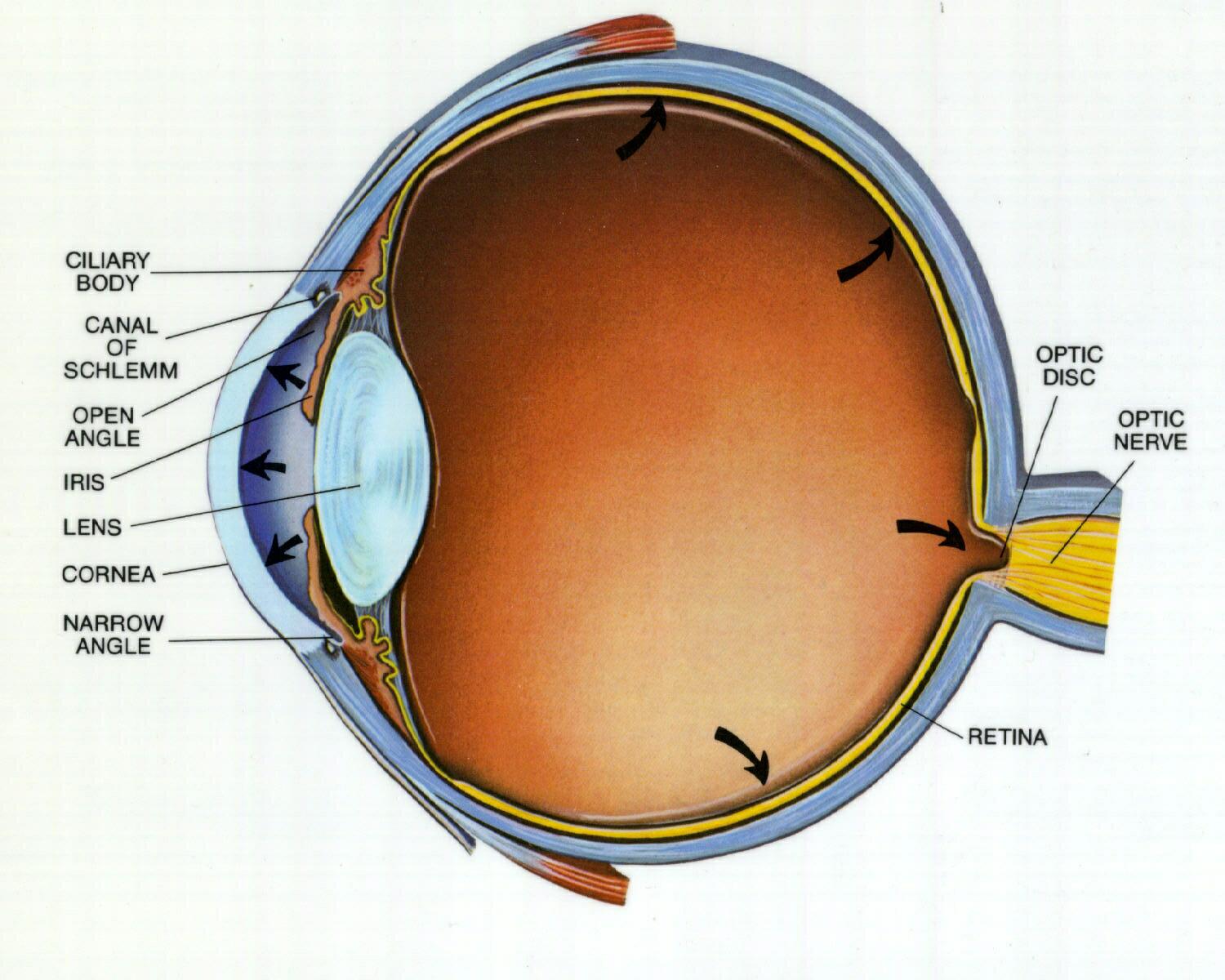
- 🚱 Due to impaired aqueous humor drainage through the trabecular meshwork, despite an “open” anterior chamber angle.
⚡ Risk Factors
- 👴 Age > 40 years
- 👨👩👦 Family history of glaucoma
- 🏿 Black ethnicity (higher risk and earlier onset)
- 👓 High myopia (short-sightedness)
- 🩸 Systemic conditions: diabetes, hypertension, thyroid disease
🔍 Clinical Presentation
- ❌ Usually asymptomatic until late disease.
- 🔴 Optic Disc Cupping: cup-to-disc ratio > 0.7, often asymmetric.
- 👁️🗨️ Visual Field Defects: classically nasal step, arcuate scotoma → progressing to tunnel vision.
- ⏳ Progression: peripheral vision lost first, central vision threatened later → untreated cases risk total blindness.
💊 Management (Target IOP < 21 mmHg)
- Topical Medications:
- 💧 Beta-Blockers (Timolol, Betaxolol): ↓ aqueous humor production. ⚠️ Avoid in asthma, COPD, bradycardia.
- 🌿 Prostaglandin Analogs (Latanoprost): ↑ aqueous outflow. Once daily; can cause iris darkening.
- 🌊 Pilocarpine: miotic agent ↑ trabecular outflow, but causes miosis → ↓ night vision & brow ache.
- 💊 Carbonic Anhydrase Inhibitors (Acetazolamide, Dorzolamide): ↓ aqueous humor production; oral forms reserved for acute/short-term use.
- Procedures:
- 🔦 Laser Trabeculoplasty (e.g., Argon): improves outflow via trabecular meshwork.
- 🔧 Trabeculectomy: creates a drainage fistula → lowers IOP. Gold standard for refractory disease.
- 🌀 Minimally Invasive Glaucoma Surgery (MIGS): newer safer options (stents, shunts) for moderate disease.
📈 Prognosis
- 🔎 With regular screening + treatment, most patients preserve useful vision for life.
- ⚠️ Untreated → progressive field loss and irreversible blindness.
- 👓 Regular monitoring of IOP, visual fields, and optic disc is essential.
📚 References
Cases - Primary Open-Angle Glaucoma (POAG)
- Case 1 - Asymptomatic detection 👓: A 62-year-old man attends a routine optician’s appointment. Intraocular pressure (IOP) 28 mmHg, optic disc shows increased cup-to-disc ratio, and visual field test reveals arcuate scotoma. He has no symptoms. Diagnosis: POAG detected on screening. Managed with topical prostaglandin analogue (latanoprost) and referral to ophthalmology.
- Case 2 - Gradual visual loss 🕶️: A 70-year-old woman reports difficulty with peripheral vision and frequent tripping. Central vision is preserved. Exam: elevated IOP, optic disc cupping, bilateral peripheral visual field loss. Diagnosis: established POAG. Managed with topical therapy (beta-blocker, prostaglandin analogue), laser trabeculoplasty if uncontrolled.
- Case 3 - Strong family history 🧬: A 55-year-old man with a father blinded by glaucoma attends for review. He is asymptomatic but has borderline raised IOP, enlarged cup-to-disc ratio, and thinning of retinal nerve fibre layer on OCT. Diagnosis: early POAG in high-risk patient. Managed with prophylactic IOP-lowering drops and lifelong surveillance.
Teaching Point 🩺: Primary open-angle glaucoma = chronic, progressive optic neuropathy due to impaired aqueous outflow → optic nerve cupping and visual field loss. Key risk factors: age, family history, African/Caribbean ethnicity, myopia, diabetes, hypertension. Insidious onset: patients often unaware until late. Management: prostaglandin analogues first-line, then beta-blockers, carbonic anhydrase inhibitors, or surgical/laser trabeculoplasty if progression.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
