Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
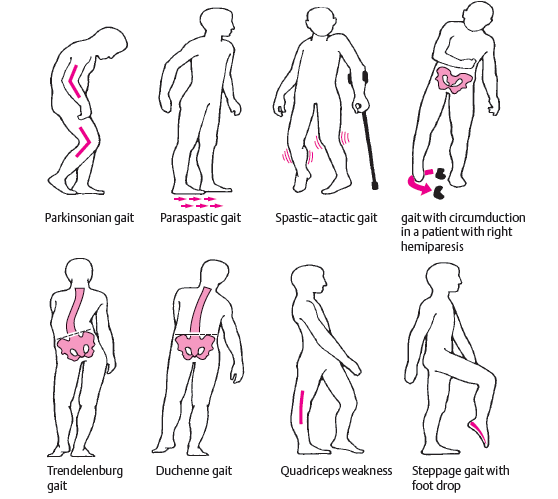
Pathological Gaits 🚶♂️
Gait is a dynamic neurological examination that integrates cortex, basal ganglia, cerebellum, brainstem, spinal cord, peripheral nerves, and muscle. Abnormal gait patterns often provide earlier and more reliable localisation than isolated power testing. In clinical practice and UK exams, recognising the gait pattern is usually more important than naming the disease.
🧠 Hemiplegic (Circumduction) Gait
This gait is caused by unilateral upper motor neuron weakness, most commonly following stroke. The affected leg is stiff and extended, swinging outward in a semicircle to clear the ground due to spasticity and reduced knee flexion. The ipsilateral arm is typically flexed and adducted.
- Cause: Corticospinal tract lesion above decussation
- Features: Stiff leg, circumduction, reduced arm swing
- Think: Stroke, brain tumour, MS, demyelination
🧠 Spastic Diplegic (Scissoring) Gait
Spasticity predominantly affects both legs, leading to hip adduction and crossing of the legs during walking. This reflects bilateral corticospinal tract involvement, often with relative sparing of the arms.
- Cause: Bilateral UMN pathology
- Features: Narrow base, legs crossing (“scissoring”)
- Think: Cerebral palsy, cervical myelopathy
🧠 Parkinsonian Gait
Parkinsonian gait reflects basal ganglia dysfunction with impaired initiation and scaling of movement. Patients walk with short, shuffling steps, reduced arm swing, and a stooped posture. Festinating gait may develop, where steps become progressively faster and shorter.
- Cause: Dopaminergic deficit in basal ganglia circuits
- Features: Shuffling, freezing, reduced arm swing
- Think: Parkinson’s disease, drug-induced parkinsonism
🎯 Cerebellar Ataxic Gait
Cerebellar disease produces a wide-based, unsteady gait with irregular steps and truncal instability. Patients appear “drunk” and may veer to one side. Visual input does not significantly improve stability, distinguishing it from sensory ataxia.
- Cause: Cerebellar hemisphere or vermis pathology
- Features: Wide base, staggering, poor tandem gait
- Think: Alcohol-related disease, stroke, tumour
🦵 Sensory Ataxic (Stamping) Gait
Loss of proprioception leads patients to rely heavily on visual input for balance. They walk with high-stepping, forceful foot placement and become markedly worse in the dark or with eyes closed. This is classically associated with a positive Romberg’s test.
- Cause: Dorsal column or peripheral nerve disease
- Features: Stamping gait, worse without visual input
- Think: Vitamin B12 deficiency, peripheral neuropathy
💪 Myopathic (Waddling) Gait
Proximal muscle weakness, particularly of the hip girdle, causes instability during single-leg stance. Patients compensate by tilting their trunk side-to-side, producing a waddling appearance. Rising from a chair or climbing stairs is often difficult.
- Cause: Proximal muscle weakness
- Features: Waddling, lordosis, difficulty standing
- Think: Muscular dystrophy, inflammatory myopathy
⚡ High-Stepping (Foot Drop) Gait
Weak ankle dorsiflexion causes the foot to drag during swing phase. Patients compensate by lifting the knee higher than normal to avoid tripping. The foot often slaps the ground on contact.
- Cause: Common peroneal nerve or L5 root lesion
- Features: High knee lift, foot slap
- Think: Peripheral neuropathy, radiculopathy
🧠 Frontal (Apraxic) Gait
Despite preserved strength, patients struggle to initiate walking and take short, hesitant steps. The gait appears “magnetic,” as if the feet are stuck to the floor. This reflects impaired motor planning rather than weakness.
- Cause: Frontal lobe or subcortical disease
- Features: Difficulty initiating gait, short steps
- Think: Normal pressure hydrocephalus, vascular dementia
🩺 Teaching Pearl
When assessing gait, ask: is the base wide or narrow, are the steps symmetric, and does vision help? Answering these three questions will usually localise the problem before you even test power. Gait is one of the highest-yield parts of the neurological examination.
🚶♂️ Pathological Gaits – Clinical Localisation Table
| Gait Pattern | Key Features | Likely Lesion | Typical Causes |
|---|---|---|---|
| Hemiplegic (Circumduction) | Stiff extended leg, swings outward; flexed adducted arm | Unilateral corticospinal tract (UMN) | Stroke, brain tumour, demyelination |
| Spastic Diplegic (Scissoring) | Narrow base, legs cross, increased tone | Bilateral corticospinal tracts | Cerebral palsy, cervical myelopathy |
| Parkinsonian | Shuffling steps, reduced arm swing, freezing, festination | Basal ganglia (dopaminergic pathways) | Parkinson’s disease, drug-induced parkinsonism |
| Cerebellar Ataxic | Wide-based, staggering, poor tandem gait | Cerebellum (vermis or hemispheres) | Alcohol-related disease, stroke, tumour |
| Sensory Ataxic (Stamping) | High-stepping, forceful foot placement, worse in dark | Dorsal columns / peripheral nerves | Vitamin B12 deficiency, neuropathy |
| Myopathic (Waddling) | Side-to-side trunk sway, difficulty standing | Proximal muscles (hip girdle) | Muscular dystrophy, inflammatory myopathy |
| High-Stepping (Foot Drop) | Excessive knee lift, foot slap | Peroneal nerve / L5 root | Peripheral neuropathy, radiculopathy |
| Frontal (Apraxic / Magnetic) | Difficulty initiating gait, short hesitant steps | Frontal lobes / subcortical circuits | Normal pressure hydrocephalus, vascular dementia |
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology