| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Altitude sickness / Acute Mountain sickness
Related Subjects: | Assessing Breathlessness | Respiratory Failure | Caisson Disease - Decompression Sickness | Altitude Sickness / Acute Mountain Sickness
🏔️ Altitude Sickness (Acute Mountain Sickness, AMS) is a condition that can occur when individuals ascend too quickly above 8,000 ft (2,500 m). ⚠️ Complications: AMS, High Altitude Pulmonary Oedema (HAPE), and High Altitude Cerebral Oedema (HACE). 🩺 Management: Stop ascent, allow acclimatisation, rest, hydrate, and descend if severe.
ℹ️ About
- Occurs with rapid ascent above ⛰️ 2,500 m
- Hypoxia → pulmonary vasoconstriction
- Causes hypocarbia + alkalosis
- Severe cases → pulmonary & cerebral oedema
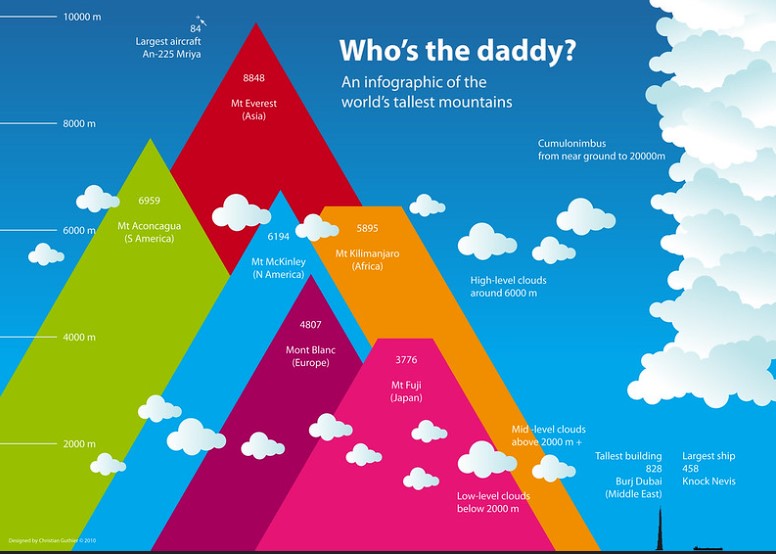
🗺️ Geography (Examples)
- 🇬🇧 Ben Nevis: 1,345 m (rare AMS)
- 🇨🇭 Matterhorn: 4,478 m
- 🇫🇷 Mont Blanc: 4,807 m
- 🌍 Kilimanjaro: 5,895 m
- 🇳🇵 Everest: 8,848 m
🧬 Aetiology
- Exaggerated vascular response to hypoxia
- Acclimatisation = adaptive molecular & cellular changes
⚠️ Severity Factors
- Rate of ascent ⏫
- Maximum altitude reached ⛰️
- Length of stay 🕒
- Physical exertion 💪
🔎 Risk Factors
- Rapid ascent, poor acclimatisation
- Altitude > 2,500 m
- 💧 Dehydration, ❄️ hypothermia
- 🍷 High alcohol intake
- 💪 Excess exertion in early days
- 📜 Hx anaemia, AMS, pulmonary/cardiac disease
🧪 Pathology
- HAPE: pulmonary oedema, alveolar haemorrhage
- HACE: cerebral oedema
- Retinal haemorrhages possible 👁️
🧾 Types
- HAPE 🫁: Breathlessness, pink frothy sputum, cyanosis
- HACE 🧠: Confusion, ataxia, coma
- AMS 🥴: Headache, nausea, dizziness, insomnia
- High altitude retinal haemorrhage 👁️: Blurred vision
🩺 Clinical Symptoms
- AMS: Headache, nausea, fatigue, insomnia, facial swelling, oliguria
- HAPE: Cough, haemoptysis, wheeze, cyanosis, basal crackles
- HACE: Severe headache, confusion, ataxia, seizures, coma
🔍 Investigations
- FBC: ↑ haematocrit / Hb
- ABG: ↓ O₂, ↓ CO₂
- ECG: sinus tachycardia ❤️
- CXR: pulmonary oedema
💊 Management
- Prevention / Avoidance ⛺:
- First night < 2,400 m
- Above 2,700 m → ascend ≤ 300 m/day
- Sleep lower than day’s highest point
- “Pole-pole” (slow pace) 🐢
- Avoid alcohol, smoking, sedatives
- Hydrate 3–4 L/day
- 💊 Diamox (acetazolamide) prophylaxis
- AMS 🥴: Rest, descent, O₂, hyperbaric bag if no descent possible
- HAPE 🫁: Rapid descent, O₂, hyperbaric chamber; nifedipine/sildenafil may help
- HACE 🧠: High-flow O₂, descent, dexamethasone 8 mg QDS, acetazolamide
📚 Reference
🧑⚕️ Case Examples - Acute Mountain Sickness (AMS)
- Case 1 (Mild AMS - headache & nausea): 🏔️ A 26-year-old hiker ascends rapidly from sea level to 3,200 m in 24 hours. Within 12 hours, he develops a throbbing headache, nausea, and poor sleep. Analysis: Rapid ascent without acclimatisation → classic trigger. Diagnosis: Lake Louise criteria: headache + GI upset + sleep disturbance = mild AMS. Management: Rest at altitude, avoid further ascent, simple analgesia, antiemetic. Monitor closely; usually self-limiting.
- Case 2 (Moderate AMS - impaired function): ⛷️ A 34-year-old skier ascends to 3,800 m. After 24 hours, he reports severe headache, dizziness, anorexia, and difficulty walking straight. Analysis: Functional impairment = moderate AMS. Risk of progression to HACE/HAPE if ascent continues. Diagnosis: Clinical (Lake Louise score >5, impaired coordination). Management: Halt ascent, give supplemental oxygen if available, acetazolamide to hasten acclimatisation, consider descent if symptoms persist >24 hours.
- Case 3 (Severe AMS with HACE progression): 🚨 A 40-year-old climber at 4,500 m develops confusion, ataxia, and vomiting after 2 days of persistent headache and insomnia. Companions note he is disoriented. Analysis: AMS progressing to High-Altitude Cerebral Edema (HACE), a life-threatening emergency. Diagnosis: Severe AMS with neurological signs = HACE. Management: Immediate descent, high-flow oxygen, dexamethasone, hyperbaric bag if descent impossible. Evacuation to lower altitude hospital.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
