| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
The Fetal Head and Vaginal Birth
📝 Overview
The position and size of the fetal head are central to the labor process. 🧠 Knowledge of skull anatomy, sutures, diameters, and cardinal movements helps in recognising normal labor vs when intervention is required.
👶 Normal (Spontaneous Vaginal) Delivery – Overview
Normal delivery refers to the natural, spontaneous birth of the baby through the vagina at term (≥ 37 weeks), following spontaneous onset of labour, without the need for operative assistance (forceps, ventouse, or caesarean section). The process occurs in three physiological stages and requires close coordination between the obstetric, midwifery, and neonatal teams. 🤝
🩺 Stage 1 – Cervical Dilatation
- Latent phase: Cervix effaces and dilates to ~4 cm. Contractions mild to moderate. Woman is supported, hydrated, and encouraged to mobilise.
- Active phase: 4–10 cm dilation with strong, regular contractions every 2–3 minutes. Monitor contractions, maternal pulse, BP, and fetal heart (CTG or Doppler). Assess progress by vaginal examination every 4 hours using a partogram. Encourage upright posture, analgesia as needed (TENS, gas & air, epidural if appropriate).
🤰 Stage 2 – Expulsion of the Fetus
- Begins at full cervical dilatation (10 cm) and ends with the birth of the baby.
- Maternal bearing-down efforts coordinated with contractions.
- Delivery sequence: Head engages → flexes → descends → rotates → extends → restitutes → shoulders and body delivered.
- The midwife supports the perineum (“hands-on” or “hands-poised”) to reduce tears.
- Check for nuchal cord (around neck) and deliver shoulders gently.
- Once born: dry and stimulate the baby, clamp and cut the cord after 1–3 minutes (delayed clamping), and place the baby skin-to-skin with mother. 🤱
- Assess Apgar scores at 1 and 5 minutes; handover to neonatal team if concerns.
🩸 Stage 3 – Delivery of the Placenta
- Begins immediately after birth of the baby and ends with expulsion of the placenta and membranes.
- Active management (standard in UK practice):
- Administer IM oxytocin (10 IU) within 1 minute of birth.
- Controlled cord traction with counter-pressure on uterus.
- Inspect placenta and membranes for completeness and cord insertion.
- Physiological management (rarely used) — no uterotonic, placenta delivered spontaneously.
- Check uterus is well-contracted to reduce haemorrhage risk.
👩⚕️ Role of the Delivery Team
- 🧑🍼 Midwife: Continuous labour support, fetal and maternal monitoring, guiding pushing, delivering baby, assessing perineum, performing active management of third stage.
- 👩⚕️ Obstetrician: Present if risk factors arise (fetal distress, malposition, slow progress, bleeding, shoulder dystocia, etc.).
- 👶 Neonatal/Paediatric Team: Standby for high-risk deliveries; immediate newborn assessment, resuscitation if required.
- 🧍 Support partner: Provides emotional support and reassurance to the mother.
✅ After Delivery
- Examine the perineum for tears and repair as needed.
- Record maternal vitals, uterine tone, and vaginal loss.
- Encourage bonding, early breastfeeding, and skin-to-skin contact. 🤱
- Observe for postpartum haemorrhage or retained tissue.
- Document time of delivery, placenta, blood loss, and Apgar scores.
💡 Teaching Tip: Always observe calm, clear communication between the team. Labour is physiological but can become high-risk in minutes — the best teams anticipate rather than react. 🌟
🦴 Bones of the Fetal Skull
- The fetal skull consists of multiple bones separated by sutures, allowing molding during birth.
- Main bones:
- 👶 Frontal bones: Forehead region.
- 👂 Parietal bones: On either side.
- 🎯 Occipital bone: Back of the head.
- ⏳ Temporal bones: Sides of the skull.
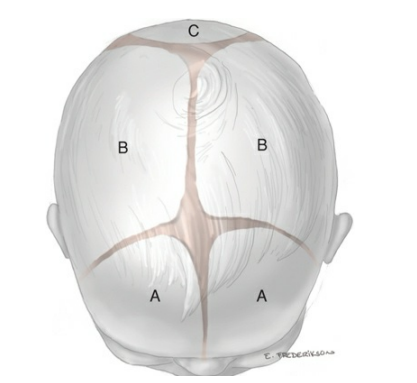
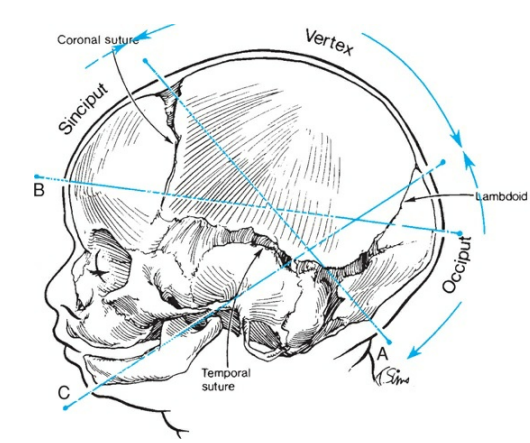
🪢 Sutures and Fontanelles
- Sutures: Flexible joints aiding molding:
- 🔹 Coronal → between frontal & parietal bones.
- 🔹 Sagittal → between parietal bones.
- 🔹 Lambdoid → between parietal & occipital bones.
- Fontanelles: Soft spots where sutures meet:
- 🔷 Anterior fontanelle: Diamond-shaped, at coronal + sagittal junction.
- 🔺 Posterior fontanelle: Triangular, at sagittal + lambdoid junction.
📏 Fetal Head Diameters in Vaginal Birth
- 📍 Suboccipitobregmatic (9.5 cm): Smallest, ideal for delivery.
- 📍 Occipitofrontal (11 cm): Flexed head presentations.
- 📍 Mentofrontal (13.5 cm): Brow presentation → obstructed labor risk.
- 📍 Submentobregmatic (9.5 cm): Face presentation.
🔄 Mechanisms of Labor (Cardinal Movements)
The fetal head adapts through a sequence of movements to navigate the pelvis:
- ⬇️ Engagement: Biparietal diameter enters pelvic brim (often occiput transverse).
- ↘️ Descent: Progression into pelvis via contractions & gravity.
- 🤰 Flexion: Chin to chest → smallest diameter presents.
- ↩️ Internal Rotation: Occiput rotates anteriorly to align with pelvis.
- ⤴️ Extension: Occiput, brow, then face emerge under pubic symphysis.
- 🔄 External Rotation (Restitution): Head realigns with shoulders.
- 👶 Expulsion: Shoulders + body delivered.
📌 Common Fetal Head Positions
- ✅ Occiput Anterior (OA): Best position → easiest passage.
- ⚠️ Occiput Posterior (OP): “Back-to-back” → prolonged labor, higher operative risk.
- ➡️ Transverse: Head sideways → may need rotation/assistance.
🚨 Complications of Malposition
- 📏 Cephalopelvic Disproportion (CPD): Head too large/poor fit with maternal pelvis.
- 😧 Face/Brow Presentation: Large diameters → obstructed labor, often C-section.
- 💡 Shoulder Dystocia: Shoulders stuck after head → emergency manoeuvres needed.
🔑 Key Points for Clinical Practice
- 🔍 Always assess fetal position & engagement early in labor.
- 🌀 Recognising abnormal progress by understanding cardinal movements guides safe decisions.
- ⏱️ Timely intervention in malposition or disproportion reduces risks for mother & baby.
📚 Mastery of fetal head anatomy, diameters, and labor mechanics equips clinicians to anticipate difficulties and manage birth safely.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
