| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
AIDS HIV Infection
Related Subjects: |AIDS (HIV) Neurological Disease |AIDS (HIV) Respiratory disease |AIDS Dementia Complex (HIV) |AIDS HIV Infection |AIDS(HIV) Gastrointestinal Disease |Acute Retroviral Syndrome (HIV) |HIV and Post-Exposure Prophylaxis (PEP) |HIV and Pre-exposure prophylaxis |HIV associated nephropathy (HIVAN) |HIV disease Assessment |Immune Reconstitution Syndrome |AIDS HAART Antiretrovirals |Kaposi sarcoma (KS)
| Algorithm — Approach to Fever in an HIV Patient (by CD4 Count) |
|---|
|
Teaching Commentary 📘
Always anchor your thinking in the CD4 count: - <200 → PCP, candidiasis. - <100 → toxoplasma, cryptococcus. - <50 → CMV, MAC, PML. But don’t forget “common things are common” — pneumonia and sepsis still outnumber rare OIs in the UK. Exams love CD4 thresholds as memory triggers, but in practice you always treat what’s in front of you. Early ART makes severe OIs much less common, but they remain vital for finals and MRCP.
🌡️ Many people with HIV have no obvious signs or symptoms. Always consider risk factors and test early.
📌 Introduction
- HIV prognosis has improved dramatically with HAART (triple therapy).
- Late diagnosis (low CD4 at presentation) worsens outcomes.
- Common causes of death now: CAD, liver failure (HBV/HCV), and lymphoma.
- HAART transforms HIV into a chronic manageable disease with near-normal life expectancy.
🦠 About the Virus
- HIV-1: Global, predominant type.
- HIV-2: Less virulent, resistant to NNRTIs, common in West Africa.
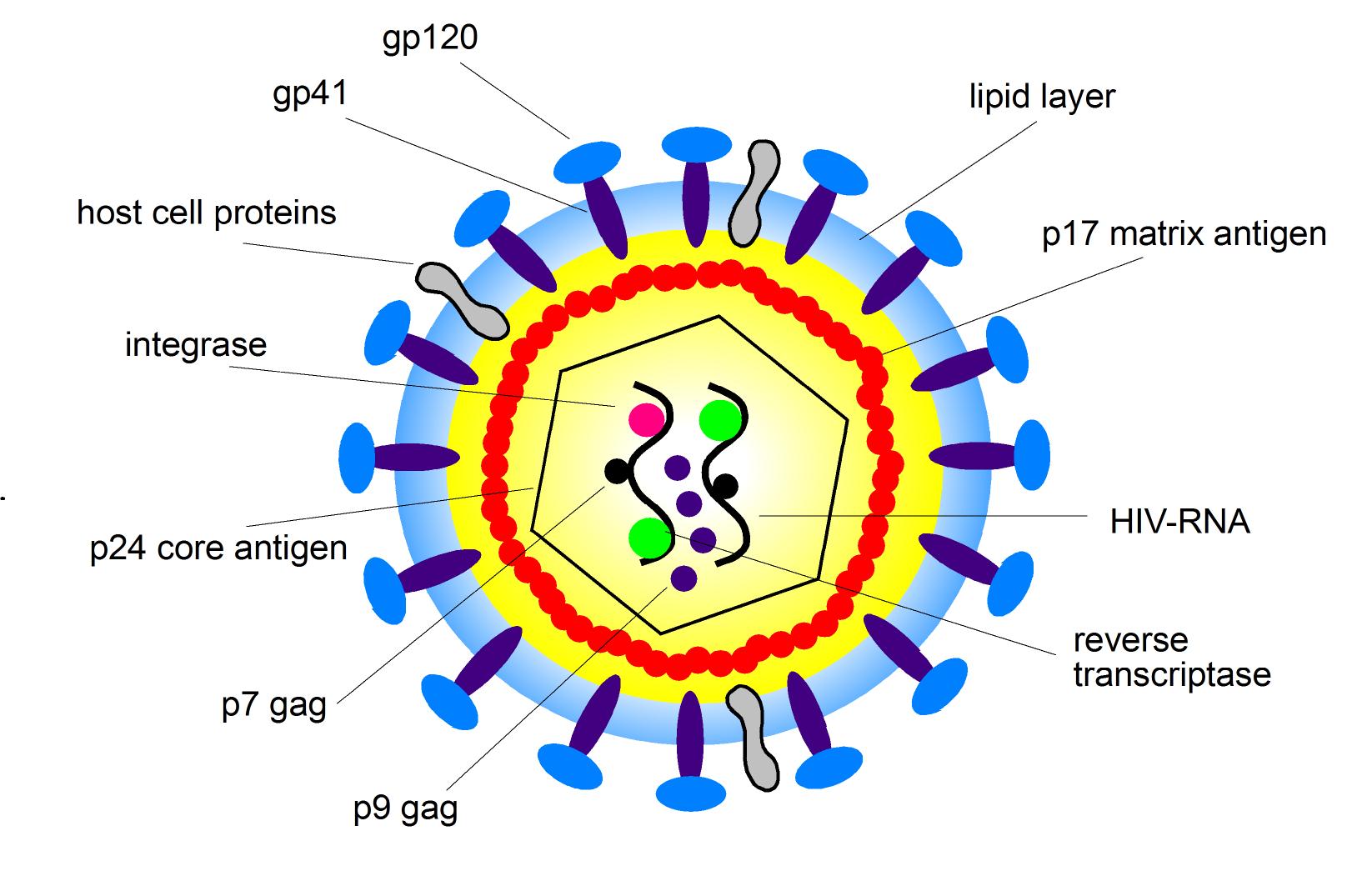
🔬 Structure
🌀 Viral Cycle
- gp120 binds CD4 → chemokine receptor (CCR5/CXCR4).
- Fusion + entry via gp41.
- RNA → DNA via reverse transcriptase.
- Integration via integrase.
- Viral proteins made by host cell machinery.
- Virions assembled → released.
🧬 Genes
- gag = structural proteins
- pol = enzymes (RT, protease, integrase)
- env = envelope glycoproteins (gp120, gp41)
- tat, rev = regulatory proteins
- vif, vpr, vpu = accessory proteins for infectivity/assembly
🎯 Tropism
- Infects CD4+ cells: T-helper cells, macrophages, dendritic cells, microglia.
- Gradual CD4 depletion → immunodeficiency.
📡 Transmission
- Sexual contact (↑ risk with concurrent STIs).
- Blood (needles, transfusions).
- Vertical: pregnancy, delivery, breastfeeding.
🌍 Epidemiology
- Worldwide burden: highest in Sub-Saharan Africa.
- HIV-1 = global; HIV-2 = mainly West Africa.
- High mutation rate → resistance challenges.
- Window period (2–6 weeks): antibody-negative but highly infectious.
🔎 Clinical Clues to Test
- Herpes zoster, unexplained lymphadenopathy.
- Paul-Bunnell negative glandular fever–like illness.
- Recurrent pneumococcal pneumonia, active TB, B-cell lymphoma.
⚠️ AIDS-Defining Conditions
- Infections: PCP, cryptococcosis, CMV, TB, MAC.
- Cancers: Kaposi’s sarcoma, invasive cervical cancer, NHL.
- Other: HIV encephalopathy, wasting syndrome.
📊 Clinical Categories
- Category A: Acute retroviral illness, PGL.
- Category B: Candidiasis, zoster >1 dermatome, hairy leukoplakia.
- Category C: AIDS-defining conditions (CD4 <200).
🧾 General Manifestations
- General: fever, wasting, anorexia.
- Liver: accelerates HBV/HCV → cirrhosis.
- Heart: myocarditis, cardiomyopathy.
- Neuro: toxoplasmosis, cryptococcal meningitis, PML.
- Skin: Kaposi’s, molluscum, seborrheic dermatitis.
- Eye: CMV retinitis, toxoplasmosis.
🧪 Investigations
- Diagnosis: ELISA → confirm with Western blot/2nd assay.
- Progression: CD4 count + viral load every 3–4 months.
- AIDS: CD4 <200 (advanced <50).
🔍 New HIV Patient Workup
- Baseline: FBC, U&E, LFT, lipids, glucose, vit D.
- Immunology: CD4, HLA-B*5701.
- Virology: viral load, subtype, HBV/HCV, syphilis.
- Screen: toxoplasmosis, cervical cytology, CXR.
🚩 Poor Prognosis Indicators
- Anaemia, thrombocytopenia.
- High HIV RNA, raised β2-microglobulin.
- CD4 <200.
💊 Management of HIV/AIDS
- 🧪 When to start ART: Current guidance = treat ALL patients, regardless of CD4 count. Earlier treatment improves outcomes, reduces transmission.
- 📉 Goals: Suppress viral load (<50 copies/mL), restore/maintain CD4 count, reduce morbidity/mortality, prevent transmission.
💊 HAART (Highly Active Antiretroviral Therapy)
- Combination of ≥3 drugs from ≥2 classes.
- Typical first-line (UK/Europe):
- 2 x NRTI backbone (e.g. tenofovir disoproxil fumarate + emtricitabine OR abacavir + lamivudine)
- + 1 integrase inhibitor (e.g. dolutegravir, bictegravir, raltegravir)
- 🛡️ Integrase inhibitors now favoured due to potency and tolerability.
📚 Drug Classes
- 🧱 NRTIs (Nucleoside RT inhibitors): Zidovudine, lamivudine, emtricitabine, tenofovir. Block reverse transcription.
- 🚫 NNRTIs: Efavirenz, rilpivirine. Bind RT at different site (resistance more likely).
- 🧲 Integrase inhibitors: Dolutegravir, bictegravir. Block viral DNA integration into host genome.
- 🔒 Protease inhibitors (PIs): Atazanavir, darunavir, ritonavir. Prevent viral protein maturation.
- 🔑 Entry/CCR5 inhibitors: Maraviroc (CCR5 antagonist).
- 🧩 Fusion inhibitor: Enfuvirtide (rarely used).
📉 Monitoring
- Check viral load + CD4 count at baseline, then at 1–3 months post-initiation, then every 3–6 months.
- Target = undetectable viral load within 6 months.
- Monitor for drug toxicity: renal (tenofovir), hepatic, lipid/glucose profile (PIs).
📌 Other Key Measures
- 🎯 Vaccination: give inactivated vaccines (e.g. influenza, pneumococcus, hepatitis B). Live vaccines usually avoided if CD4 <200.
- 🍼 Preventing mother-to-child transmission: ART in pregnancy + neonatal prophylaxis + avoid breastfeeding if safe alternative exists.
- ❤️ Sexual transmission: ART reduces transmission risk to near zero if viral load is suppressed (“U=U”).
- 💉 Post-exposure prophylaxis (PEP): 28 days of ART after high-risk exposure (e.g. needlestick, unprotected sex). Best started <72 hrs.
- 🧪 Pre-exposure prophylaxis (PrEP): Tenofovir + emtricitabine daily in high-risk individuals (e.g. MSM, serodiscordant couples).
⚠️ When to use Steroids
- Cryptococcal meningitis: avoid (may worsen outcome).
- PCP with hypoxia: Prednisolone as adjunct therapy.
- Immune Reconstitution Inflammatory Syndrome (IRIS): May require corticosteroids if severe.
CD4 Count Thresholds and Opportunistic Infections in HIV
| CD4 Count | Common Opportunistic Infections | Prophylaxis / Notes |
|---|---|---|
| <500 |
|
No routine prophylaxis; start ART. |
| <200 |
|
Co-trimoxazole daily for PCP prophylaxis (stop once CD4 >200 on ART). |
| <100 |
|
Co-trimoxazole also covers toxoplasmosis (if IgG+). Consider fluconazole prophylaxis in high-risk settings. |
| <50 |
|
Azithromycin or clarithromycin weekly for MAC prophylaxis (if ART delayed). Regular fundoscopy for CMV monitoring. |
Teaching Commentary 🧬
Declining CD4 count predicts vulnerability to specific infections. The big exam clue is: - <200 → think PCP, - <100 → think toxoplasmosis, cryptococcus, - <50 → think CMV and MAC. In modern UK/European practice, early ART makes these rare, but they remain core exam topics. Always combine OIs treatment + ART + prophylaxis. Remember to stop prophylaxis once CD4 has recovered >200 for >3–6 months on ART.
Cases — HIV / AIDS
- Case 1 — Primary HIV Infection (Seroconversion Illness): A 23-year-old man presents with 2 weeks of fever, sore throat, rash, and lymphadenopathy after unprotected sex abroad. HIV antibody/antigen test positive. Diagnosis: Acute HIV seroconversion illness. Management: Baseline CD4/viral load; start ART promptly; screen for co-infections (HBV, HCV, syphilis, TB).
- Case 2 — Oral Candidiasis in Untreated HIV: A 32-year-old woman with known HIV not on therapy presents with dysphagia and white plaques on her tongue. CD4 count 180. Diagnosis: Oropharyngeal/esophageal candidiasis (AIDS-defining when oesophageal). Management: Oral fluconazole; initiate ART.
- Case 3 — Pneumocystis jirovecii Pneumonia (PCP): A 41-year-old man with untreated HIV presents with progressive dyspnoea, dry cough, and fever. O₂ sats 90% on air. CXR: bilateral interstitial infiltrates. CD4 count 90. Diagnosis: PCP pneumonia. Management: High-dose co-trimoxazole ± corticosteroids (if hypoxic); oxygen; start ART after acute infection stabilises; PCP prophylaxis if CD4 <200.
- Case 4 — Cerebral Toxoplasmosis: A 37-year-old woman with HIV presents with new-onset seizures and confusion. MRI brain: multiple ring-enhancing lesions. CD4 count 50. Diagnosis: Cerebral toxoplasmosis. Management: Pyrimethamine + sulfadiazine + folinic acid; ART; seizure control.
- Case 5 — Kaposi’s Sarcoma (AIDS-Defining Cancer): A 45-year-old man presents with multiple purple nodular skin lesions on his legs and palate. CD4 count 120. Diagnosis: Kaposi’s sarcoma (HHV-8 related). Management: Start ART; chemotherapy if widespread or visceral involvement.
Teaching Commentary 🧬
HIV infection progresses through: 1. Primary infection (flu-like seroconversion illness), 2. Asymptomatic chronic stage (may last years), 3. Symptomatic HIV (opportunistic infections when CD4 falls), 4. AIDS (CD4 <200 or AIDS-defining illness). Key opportunistic infections: PCP, toxoplasmosis, CMV, candidiasis, cryptococcosis. AIDS-defining cancers: Kaposi’s sarcoma, NHL, cervical carcinoma. Management = prompt ART for all patients, prophylaxis against OIs, treatment of complications, and multidisciplinary care (ID, oncology, mental health, social support).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
