| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Brain Tumours in Children
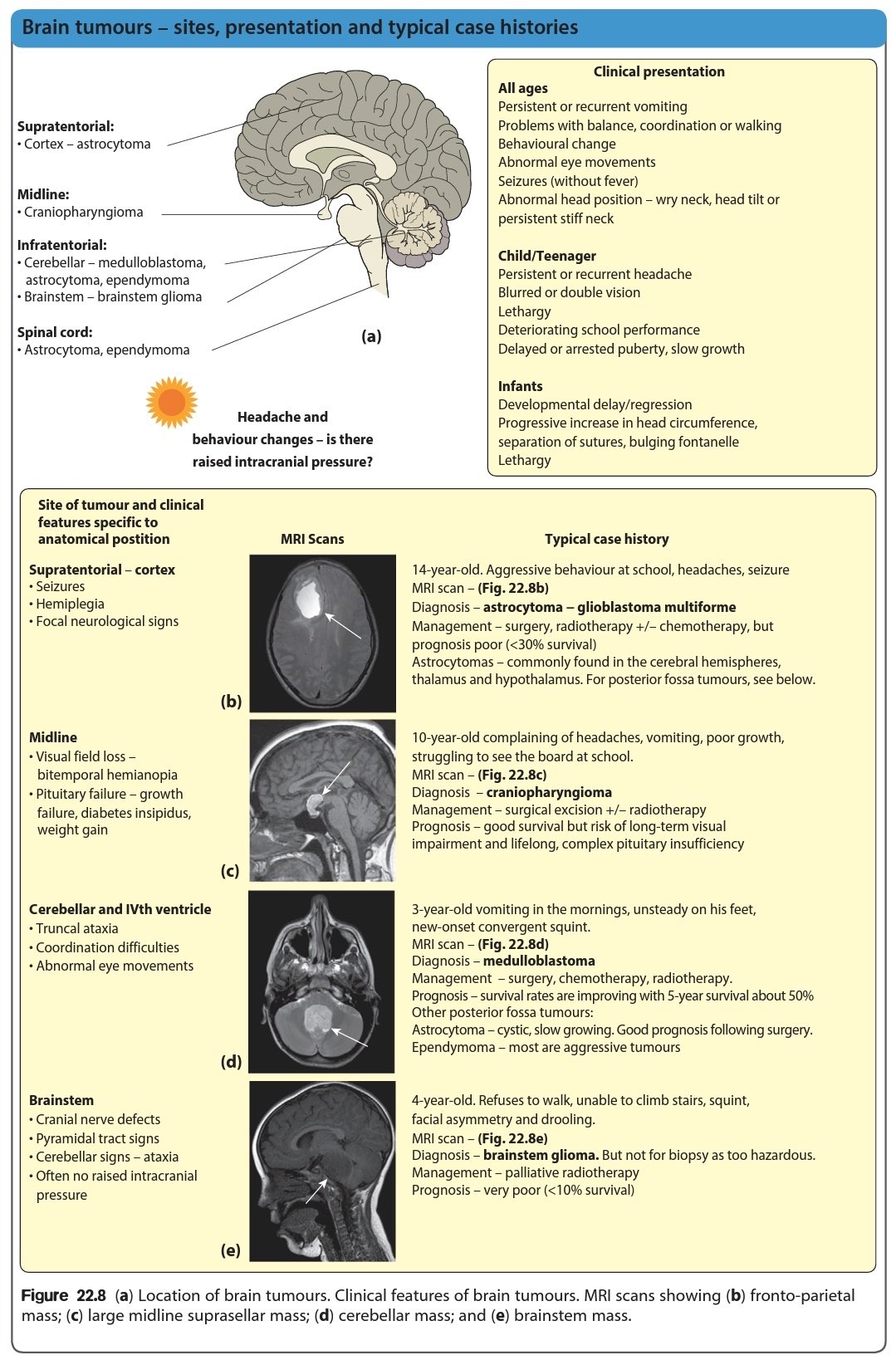
🧠 Brain tumours are the most common solid tumours in children, making up ~20% of childhood cancers. They can occur in the cerebrum, cerebellum, brainstem, or spinal cord, producing diverse symptoms depending on location and size. ✨ Advances in imaging, neurosurgery, radiotherapy, and chemotherapy have significantly improved survival and quality of life in many children.
📊 Common Types of Paediatric Brain Tumours
- Medulloblastoma: Fast-growing tumour in the cerebellum, causing gait imbalance and raised ICP. Most common malignant brain tumour in children.
- Pilocytic Astrocytoma (low-grade astrocytoma): Usually benign, slow-growing, and often curable with surgery. Often arises in the cerebellum or optic pathway.
- Ependymoma: Originates from ependymal cells lining the ventricles; can obstruct CSF flow → hydrocephalus.
- Brainstem Glioma: Includes DIPG, aggressive and inoperable, affecting cranial nerves, swallowing, and breathing.
- Craniopharyngioma: Benign but locally invasive tumour near the pituitary gland, leading to endocrine dysfunction and visual loss.
⚠️ Symptoms (depend on location & size)
- 🌅 Morning headaches (↑ intracranial pressure)
- 🤢 Nausea & vomiting
- 👀 Vision or hearing changes
- 🤸 Problems with balance or coordination
- ⚡ Seizures
- 🧩 Behavioural or cognitive decline (school performance issues)
- 👶 In infants: bulging fontanelle, increasing head circumference
🔍 Diagnosis
- Neuroimaging: MRI (preferred) ± CT for acute hydrocephalus.
- Neurological exam: Cranial nerves, motor, gait, fundoscopy (papilloedema).
- Biopsy: Histology & molecular profiling guide treatment.
- Multidisciplinary team: Paediatric oncologists, neurosurgeons, radiologists, endocrinologists, neurologists.
💊 Treatment Options
- 🛠️ Surgery: Aim for maximal safe resection to relieve mass effect and obtain histology.
- ☢️ Radiotherapy: Effective but long-term effects (endocrine, neurocognitive) limit use in <12 years. Proton therapy is emerging to reduce toxicity.
- 💉 Chemotherapy: Used in medulloblastoma, high-grade gliomas, or to delay radiotherapy in young children.
- 🎯 Targeted Therapy: E.g., BRAF inhibitors for BRAF-mutant gliomas; immune checkpoint inhibitors under study.
- 🤝 Supportive Care: Dexamethasone for raised ICP, ventriculoperitoneal (VP) shunt for hydrocephalus, physiotherapy, occupational/speech therapy, school reintegration support.
📈 Prognosis
- Pilocytic astrocytoma: Excellent survival with complete excision (>90%).
- Medulloblastoma: ~70% 5-year survival with surgery + craniospinal irradiation + chemo.
- DIPG: Poor prognosis; median survival ~9–12 months despite therapy.
- Ependymoma: Variable; outcome depends on resectability and molecular subtype.
- Craniopharyngioma: Benign but recurrent; long-term endocrine & visual morbidity common.
⚠️ Complications
- Hydrocephalus → may require VP shunt/ETV.
- Neurocognitive impairment from tumour or therapy.
- Endocrine dysfunction (growth hormone, thyroid, adrenal, puberty issues).
- Secondary malignancy post-radiotherapy.
🔬 Outlook & Research
- Genomic profiling → more precise therapy.
- Trials on immunotherapy & tumour vaccines.
- Focus on reducing long-term neurocognitive & endocrine sequelae.
📚 References
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
