| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Pericardial Effusion and Tamponade
💉 In cases of cardiac tamponade the fffusion raises the intrapericardial pressure, reducing ventricular filling and decreasing cardiac output, which can rapidly lead to cardiac arrest, rapid pericardial decompression is life-saving. Beck's triad (↑ JVP, muffled heart sounds, hypotension) must be known or arrest 🩺 Point-of-care echocardiography aids diagnosis, while emergency measures such as resuscitative thoracotomy or ultrasound-guided pericardiocentesis may be essential.
📖 Overview of Pericardial Effusion
- 💧 Pericardial effusion = accumulation of fluid in the pericardial cavity (serous, blood, pus, or chyle).
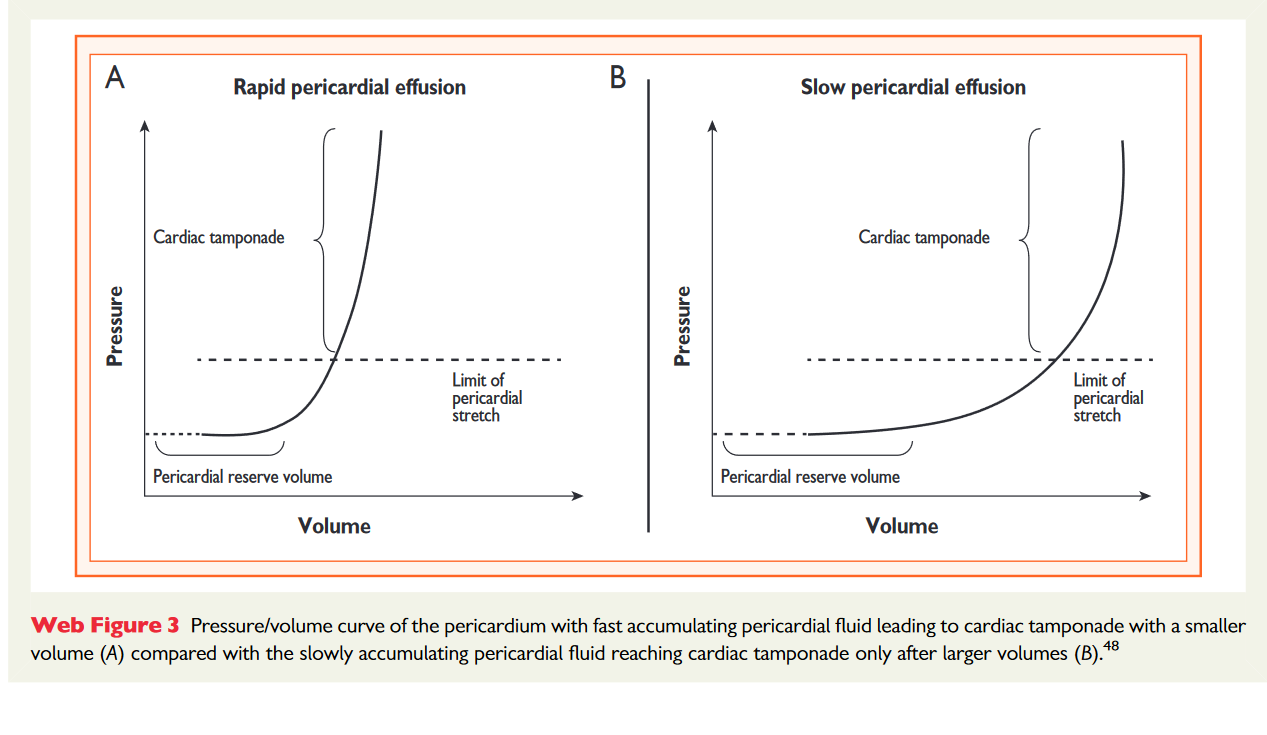
- ⚖️ Small, slow effusions may be asymptomatic, while rapid or large collections → ⛔ tamponade.
- Normal sac: 10–50 ml; can expand massively before symptoms if gradual.
- Rapid accumulation → ↑ pericardial pressure → impaired diastolic filling → ↓ cardiac output → tamponade.
🩺 Aetiology
- Normal pericardial fluid: 10–50 ml.
- Pathological effusion causes:
- 🦠 Infections: TB, viral (Coxsackie), bacterial.
- 🔥 Autoimmune: RA, lupus, scleroderma.
- 🎗️ Neoplastic: Lung, breast, melanoma.
- 💔 Post-cardiac injury: MI (Dressler’s), surgery, trauma.
- ⚠️ Other: Uraemia, hypothyroidism, aortic dissection, radiotherapy.
📊 Classification of Effusion
- ⏱️ Time: Acute/Subacute (<3 months), Chronic (>3 months).
- 📍 Distribution: Circumferential vs Loculated.
- 🫀 Haemodynamic Impact: None, Tamponade, Effusive-Constrictive.
- 🧪 Composition: Exudate, Transudate, Blood, Air/Gas.
- 📐 Size: Mild (<10 mm), Moderate (10–20 mm), Large (>20 mm).
⚠️ Causes of Pericardial Effusion & Tamponade
- 🚑 Trauma (accidents, procedures).
- 🔪 Post-surgical complications.
- 🦠 Tuberculosis (common in endemic regions).
- 🎗️ Malignancies (lung, breast, melanoma, lymphoma).
- 🩸 Aortic dissection with leakage.
- 💔 Post-MI wall rupture (3–10 days).
- 🔥 Autoimmune / renal failure (uraemic pericarditis).
👩⚕️ Clinical Presentation (Without Tamponade)
- General: Cough, fatigue, palpitations, anorexia.
- Respiratory: Dyspnoea, orthopnoea, PND.
- Systemic: Fever, malaise, features of TB/malignancy.
- Pressure effects: Hoarseness, dysphagia, nausea.
💡 Pulsus paradoxus: Pulse weakens on inspiration (SBP drop >10 mmHg).
make sure that you have considered and excluded PE, MI, Type A aortic dissection, tension pneumothorax
🚨 Clinical Presentation of Cardiac Tamponade
- Symptoms: Severe dyspnoea, chest discomfort, shock.
- Beck’s Triad:
- ↑ JVP (distended neck veins).
- ↓ BP (hypotension).
- 💤 Muffled heart sounds.
- Absent Y descent, common in TB/malignancy.
- Pulsus paradoxus (SBP fall >10 mmHg on inspiration).
- Ewart’s sign: Bronchial breath sounds at left base (compression).
- Kussmaul’s sign absent (present in constrictive pericarditis).
🔎 Investigations
- Bloods: CBC, CRP/ESR, U&E, TFTs, coagulation.
- ECG: Low voltage, tachycardia, electrical alternans.
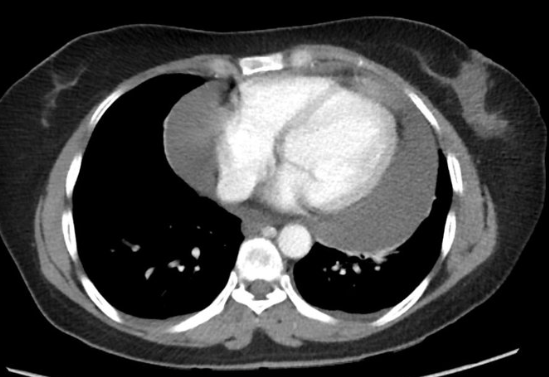
- CXR: “Water-bottle” silhouette in large effusions.
- Echocardiography: Gold standard → effusion, chamber collapse, dilated IVC. Echo-free zone around heart, diastolic collapse of the RA and RV, swinging of heart
- CT/CMR: Useful for loculated effusions or thickening.
- Fluid analysis: Gram stain, AFB, PCR, cytology, tumour markers.
💊 Management of Effusion & Tamponade
Important: Pericardiocentesis should be ultrasound-guided where available. 🎥 Watch a video guide here.
- 🚨 Emergency: ABCs, cautious IV fluids, urgent pericardiocentesis if tamponade.
- 🩺 Pericardiocentesis: Subxiphoid approach → left shoulder; catheter may be left for drainage.
- 💊 Medical therapy: NSAIDs, colchicine ± corticosteroids if inflammatory cause (exclude infection first).
- 🔪 Surgical: Pericardiectomy or pericardial window for recurrent/loculated effusions.
🩺 Case 1 — Subacute Pericardial Effusion
A 55-year-old woman with metastatic breast cancer presents with progressive breathlessness and fatigue. Examination reveals raised JVP, muffled heart sounds, and mild ankle oedema. Echocardiography shows a large pericardial effusion without chamber collapse. Management: 🩺 Treat underlying malignancy; monitor haemodynamics; pericardiocentesis or surgical pericardial window if symptomatic or haemodynamic compromise develops. Avoid: ❌ Routine diuretics (can reduce preload and precipitate tamponade). Avoid anticoagulation unless strongly indicated as it may increase risk of haemopericardium.
🩺 Case 2 — Acute Cardiac Tamponade
A 72-year-old man presents after a type A aortic dissection repair. He becomes acutely hypotensive, tachycardic, with raised JVP and muffled heart sounds (Beck’s triad). Echocardiography confirms pericardial tamponade with right atrial collapse. Management: 🚨 Emergency pericardiocentesis (if unstable and surgical delay) or immediate surgical exploration; IV fluids to maintain preload while awaiting intervention; oxygen and monitoring. Avoid: ❌ Positive pressure ventilation (reduces venous return) unless absolutely necessary. Avoid delaying definitive drainage — in tamponade this is rapidly fatal.
🩺 Case 3 — Haemopericardium on Anticoagulation
A 76-year-old woman with permanent atrial fibrillation on apixaban presents with sudden onset chest tightness, dyspnoea, and light-headedness. On exam she is tachycardic, hypotensive, with raised JVP and muffled heart sounds. Echocardiography demonstrates a large pericardial effusion with diastolic right atrial collapse, consistent with tamponade due to spontaneous haemopericardium. Management: 🚨 Immediate reversal of DOAC (andexanet alfa if available, otherwise PCC in emergencies), urgent pericardiocentesis for haemodynamic stabilisation, and cardiology input for anticoagulation strategy going forward. Supportive IV fluids and oxygen as bridge. Avoid: ❌ Continuing anticoagulation without reversal; avoid excessive diuresis (drops preload); avoid delays to drainage as tamponade physiology is life-threatening.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
