| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Monoclonal gammopathy Undetermined significance
Related Subjects: |Hypercalcaemia |Multiple Myeloma |Extramedullary Plasmacytoma |Smouldering Myeloma |MGUS |Waldenstrom Macroglobulinaemia |Oncological emergencies
🧪 Monoclonal Gammopathy of Undetermined Significance (MGUS) is a benign paraproteinaemia defined by a serum monoclonal protein < 30 g/L, < 10% plasma cells in the marrow, and no end-organ damage (CRAB: hyperCalcaemia, Renal failure, Anaemia, Bone lesions). The key differentiating feature from myeloma is the absence of complications such as immune paresis, hypercalcaemia, renal impairment, or bone disease.
📖 About
- MGUS is a paraproteinaemia that may progress to myeloma.
- Serum monoclonal protein < 30 g/L, plasma cells < 10%.
- Progression to myeloma may take years (≈1% per year risk).
📊 Epidemiology
- Asymptomatic and very common in older adults.
- ~1% prevalence over age 25, 3% >70 yrs, 10% >80 yrs.
- Only ~25% of cases progress to myeloma.
🔎 Differential Diagnosis of a Monoclonal Band
- 🦴 Multiple Myeloma: Bone pain, lytic lesions, hypercalcaemia, renal disease.
- 🧬 Lymphoma: Lymphadenopathy, hepatosplenomegaly.
- 🧪 Chronic Lymphocytic Leukaemia (CLL): Raised lymphocyte count.
- 🟢 MGUS: Asymptomatic, low paraprotein, no CRAB features.
⚡ Clinical Features
- Typically none due to MGUS itself.
- No bone pain or recurrent infections.
- 10–30% may have a demyelinating neuropathy.
🚫 In MGUS there is NO:
- Bence-Jones proteinuria.
- Lytic bone lesions.
- Hypercalcaemia.
- Renal insufficiency.
- Anaemia.
- Monoclonal Ig level > 30 g/L.
- Plasma cells > 10% on bone marrow exam.
- Immunoparesis (suppression of other Ig classes).
📈 Risk of Progression
- ~1% of patients progress to myeloma each year.
- Risk factors for progression include paraprotein type and level, and serum free light chain ratio.
🧮 Risk Stratification – “Mayo Model”
- Paraprotein > 15 g/L ➕ 1 point.
- Abnormal free light chain ratio ➕ 1 point.
- Non-IgG paraprotein (IgA, IgM, IgE) ➕ 1 point.
📊 20-Year Risk of Progression
- 0 factors → 5%.
- 1 factor → 21%.
- 2 factors → 37%.
- 3 factors → 58%.
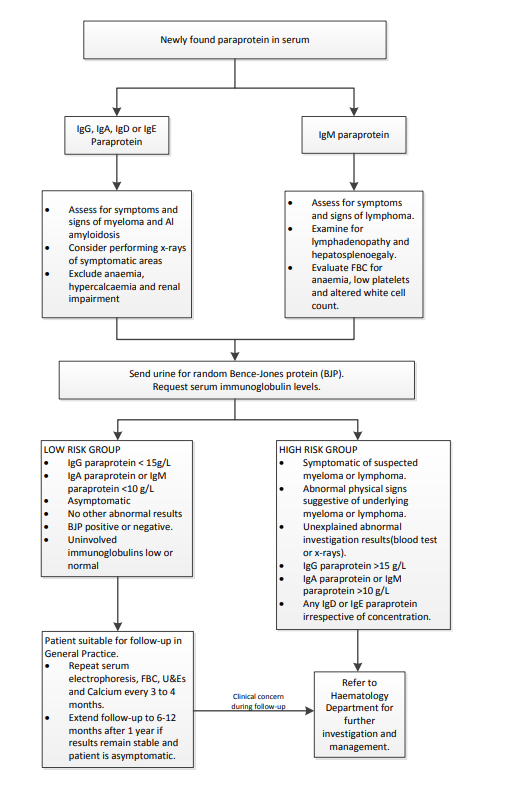
🧾 Management
- Low-risk MGUS (0–1 risk factors) can be managed in primary care.
- Follow-up every 6–12 months:
- History: weight loss, night sweats, bone pain.
- Examination: lymphadenopathy, hepatosplenomegaly.
- Tests: FBC, calcium, creatinine, albumin, SPE with paraprotein quantification.
- Refer to haematology if:
- Lymphadenopathy.
- Significant paraprotein rise (>25% & absolute rise >5 g/L).
- New cytopenias (anaemia, neutropenia, thrombocytopenia).
- Renal impairment or new bone pain.