| Download the app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. |
Giardiasis
📌 About
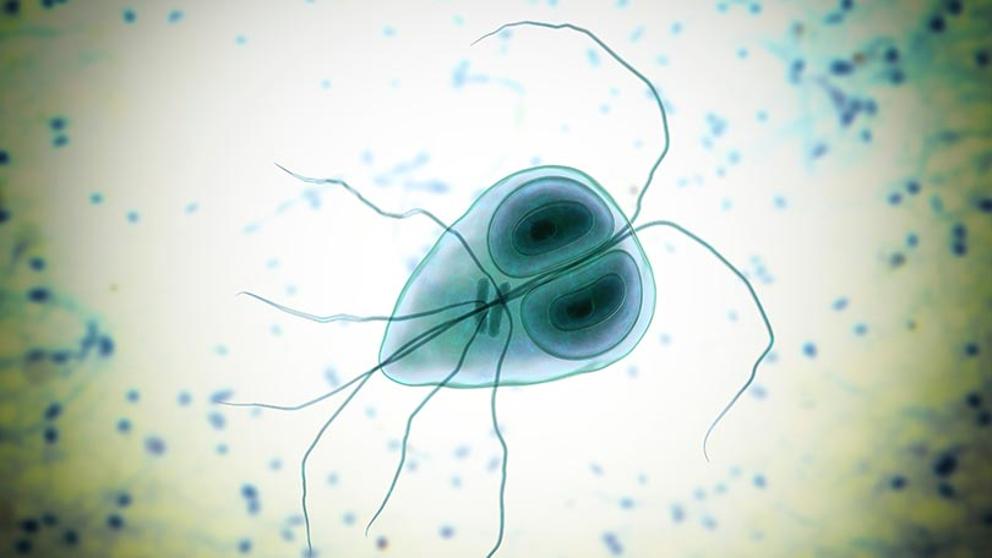
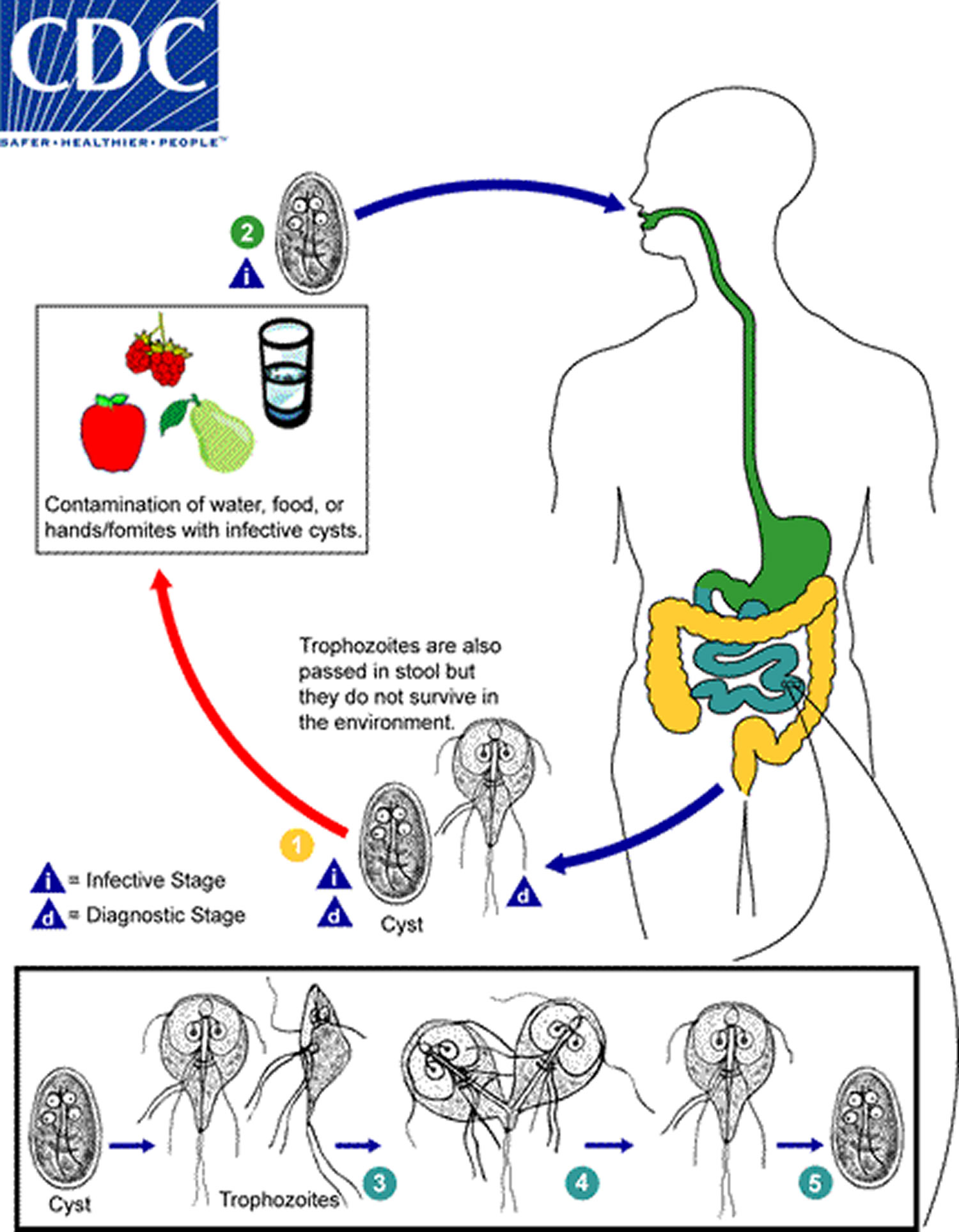
- Giardiasis is caused by the protozoan Giardia lamblia (also known as G. intestinalis).
- Exists in two forms: 🥚 cyst (infective, environmentally resistant) and 🪱 trophozoite (motile, pathogenic).
- Transmission is faeco-oral via contaminated water/food or person-to-person contact (common in nurseries, travel, camping).
- Higher risk in those with immunodeficiency (esp. IgA deficiency) or low gastric acid (e.g. PPI use).
🧬 Aetiology & Pathophysiology
- Trophozoites attach to the duodenal and jejunal mucosa via a ventral sucking disc.
- They do not invade the mucosa, but interfere with absorption → villous atrophy & enzyme deficiency (e.g. lactase deficiency).
- This causes fat and carbohydrate malabsorption → steatorrhoea and bloating.
🤒 Clinical Presentation
- Ranges from asymptomatic carriage to chronic diarrhoeal illness.
- Acute infection: watery diarrhoea, nausea, bloating, abdominal cramps.
- Chronic infection: steatorrhoea, malabsorption, weight loss, fatigue.
- Can mimic IBS or coeliac disease (“post-giardiasis lactose intolerance” may persist).
🔍 Investigations
- 📉 Bloods: low folate, low albumin, iron-deficiency anaemia in chronic disease.
- 🔬 Stool microscopy or antigen detection: cysts/trophozoites (multiple samples ↑ yield).
- 💡 Duodenal aspirates at OGD may show trophozoites.
- Biopsy: partial villous atrophy (can mimic coeliac disease, but serology negative).
💊 Management
- Metronidazole 2 g OD for 3 days (or 400 mg TDS for 5 days).
- Alternative: Tinidazole (single dose) or Nitazoxanide (3-day course).
- Treat household/close contacts if recurrent cases.
- Supportive: hydration, nutritional replacement, avoid lactose if symptomatic.
🛡️ Prevention
- Boil/filter water when travelling/camping.
- Hand hygiene in nurseries and healthcare settings.
- Avoid swimming pools if symptomatic (Giardia cysts survive chlorination).
💡 Teaching Pearls
- Giardia is the most common cause of protozoal diarrhoea in the UK (often in travellers and hikers).
- Always think of Giardia in chronic diarrhoea + bloating + weight loss with negative coeliac screen.
- Post-infective lactose intolerance may persist even after eradication.
Cases — Giardiasis
- Case 1 — Traveller’s Diarrhoea: A 26-year-old backpacker returns from Nepal with 3 weeks of foul-smelling, greasy diarrhoea, bloating, and abdominal cramps. No blood in stool. Stool microscopy: cysts of Giardia lamblia. Diagnosis: Giardiasis causing malabsorptive diarrhoea. Management: Oral metronidazole for 5–7 days; advise on hand hygiene and avoiding contaminated water.
- Case 2 — Child with Growth Faltering: A 6-year-old boy presents with chronic diarrhoea, poor weight gain, and iron deficiency anaemia. Parents note his stools are pale and difficult to flush. Stool antigen test positive for *Giardia*. Diagnosis: Chronic giardiasis with malabsorption. Management: Metronidazole or tinidazole; nutritional support; screen household contacts.
- Case 3 — Immunocompromised Patient: A 40-year-old man with untreated HIV presents with persistent watery diarrhoea, dehydration, and fatigue. Stool ELISA positive for *Giardia lamblia*. Diagnosis: Severe giardiasis in immunocompromised host. Management: Longer course of metronidazole (or nitazoxanide); optimise HIV therapy; rehydration and electrolyte replacement.
Teaching Commentary 💧
Giardiasis is a protozoal infection caused by Giardia lamblia, transmitted by ingestion of cysts in contaminated water/food or person-to-person. It classically causes foul-smelling, greasy diarrhoea, bloating, flatulence, and weight loss due to fat malabsorption. Diagnosis: stool microscopy (cysts/trophozoites), stool antigen testing, or PCR. Treatment: first-line metronidazole (or tinidazole/nitazoxanide). Relapses are common; consider treating asymptomatic carriers in households. Prevention: boil/filter water in endemic regions, good hand hygiene.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Disease
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
