Peripheral neuropathy
Note 📝:
In the UK and US, the most common causes of peripheral neuropathy are diabetes and alcohol abuse 🍺.
Worldwide 🌍, leprosy 🧑⚕️ remains a significant cause.
🔎 About Peripheral Neuropathy
- Also see “Length-Dependent Polyneuropathy” for further detail.
- Peripheral neuropathy = disease of peripheral nerves, usually secondary to systemic or primary neurological conditions.
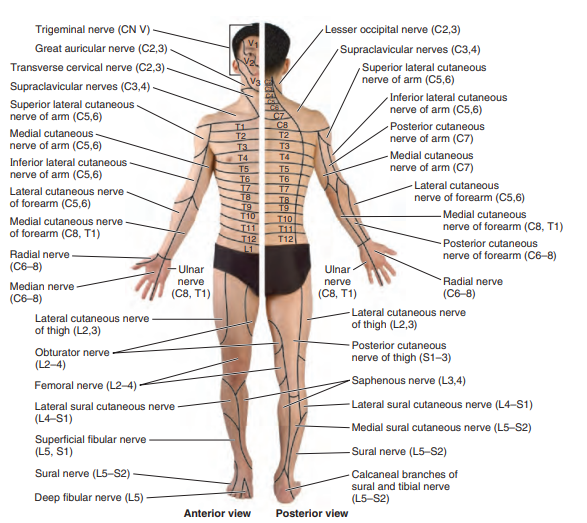
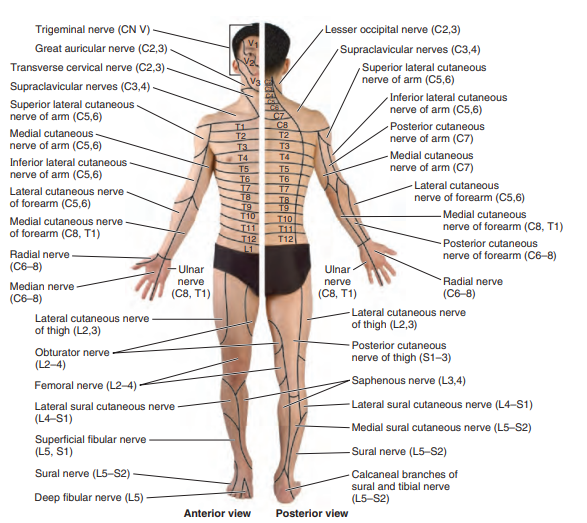
- Clinical patterns vary: may be symmetrical or patchy, distal or proximal, and affect motor, sensory, or autonomic function.
⚙️ Aetiology
- Peripheral nerves have two major fibre types:
- Small fibres 🔥: pain, temperature, autonomic function.
- Large fibres 🎻: motor strength, vibration, proprioception.
🧩 Different Forms of Peripheral Neuropathy
| Type | Description |
|---|
| Wallerian Degeneration | After nerve transection, distal axon + myelin degenerate; regeneration proceeds proximally → distally (often incomplete). |
| Axonal Degeneration | “Dying back” pattern; toxins, diabetes, alcohol, nutritional deficiencies common culprits. |
| Demyelination | Loss of myelin with preserved axons; e.g. Guillain–Barré, CIDP. |
| Neuronal Cell Body Disease | Anterior horn cell involvement (e.g. polio, MND, paraneoplastic). |
| Dorsal Root Ganglionopathy | Affects sensory ganglia; causes patchy sensory loss (e.g. paraneoplastic, Sjögren’s). |
🧭 Patterns of Peripheral Neuropathy
| Pattern | Description |
|---|
| Polyneuropathy 🧦 | Distal, symmetrical “glove and stocking” loss; diabetes, alcohol, B12 deficiency, Lyme disease. |
| Mononeuropathy 🔒 | Single nerve lesion (e.g. carpal tunnel, ulnar palsy, diabetic entrapments). |
| Mononeuritis Multiplex 🌿 | Asymmetric multi-nerve involvement; think vasculitis. |
| Autonomic Neuropathy ⚡ | Postural hypotension, bowel/bladder issues; causes include diabetes, amyloidosis, toxins. |
| Abrupt-Onset Neuropathy 🚨 | Ischaemic; PAN, RA, HIV-related. |
| Cranial Nerve Involvement 👁️ | E.g. bilateral facial palsy in diabetes, Lyme, sarcoid, GBS. |
🩺 Common Causes
| Cause | Description |
|---|
| Diabetes Mellitus | Symmetrical distal sensorimotor + autonomic neuropathy (most common UK cause). |
| Alcohol Abuse 🍺 | Painful, distal symmetric sensorimotor neuropathy; worsened by vitamin deficiencies. |
| B12 Deficiency 🍊 | Loss of proprioception, ataxia, brisk reflexes (mixed neuropathy + myelopathy). |
| Uraemia 💧 | Common in CKD or dialysis patients. |
| Autoimmune (RA, SLE) | Can cause distal sensory-motor neuropathy. |
| Paraneoplastic 🧬 | Often sensory; think lymphoma, lung cancer. |
| Vasculitis | Mononeuritis multiplex; painful, abrupt onset. |
| Chemotherapy 💊 | Platinum agents, vinca alkaloids; distal symmetrical neuropathy. |
| Guillain–Barré (GBS) | Acute demyelinating polyneuropathy with autonomic features; albuminocytologic dissociation. |
| CIDP | Chronic demyelinating sensorimotor neuropathy; relapsing/progressive course. |
| Hereditary (e.g. CMT) | Distal weakness, pes cavus, family history. |
| Leprosy 🦠 | Worldwide leading cause; thickened nerves, anaesthetic skin patches. |
🧾 Clinical Features
- Sensory: Paraesthesia, burning pain, allodynia, proprioceptive loss → ataxia.
- Motor: Distal weakness, areflexia, foot drop, “high-stepping” gait.
- Autonomic: Postural hypotension, bowel/bladder dysfunction, erectile difficulties.
- Hereditary Clues: Pes cavus, hammer toes.
- Nerve Thickening: Rare; in leprosy, CIDP, CMT.
📈 Rate of Onset
- Days: GBS, vasculitis.
- Weeks: CIDP.
- Months–Years: Diabetes, alcohol, hereditary neuropathies.
🧭 Diagnostic Clues
- Speed of onset (acute vs chronic).
- Systemic history (diabetes, alcohol, autoimmune disease).
- Cranial/autonomic involvement → red flag.
- Distribution: small fibre vs large fibre.
- Family history → hereditary cause.
🔬 Investigations
- First-line: FBC, ESR, CRP, U&E, LFTs, glucose/HbA1c, B12, folate, TFTs.
- Autoimmune: ANA, dsDNA, ENA, ANCA.
- Infectious: HIV, hepatitis serology, CXR (TB/sarcoid).
- NCS/EMG: To classify as axonal vs demyelinating, motor vs sensory.
- Selective: CSF (GBS/CIDP), ACE (sarcoid), genetic testing (CMT), nerve biopsy if unclear.
💊 Management
- Always treat the underlying cause (e.g. glycaemic control, alcohol cessation, B12 replacement).
- Neuropathic pain: duloxetine, gabapentin, pregabalin.
- Supportive: physiotherapy, orthotics, podiatry, lifestyle adjustments.
- Immune-mediated: IVIG, steroids, plasma exchange (GBS, CIDP).
Cases — Peripheral Neuropathy
- Case 1 — Diabetic Neuropathy (Metabolic):
A 62-year-old man with poorly controlled type 2 diabetes reports numbness and burning pain in both feet, worse at night. Exam: stocking distribution sensory loss, reduced ankle reflexes, preserved power.
Diagnosis: Distal symmetric sensory neuropathy due to diabetes.
Management: Optimise glycaemic control; neuropathic pain agents (duloxetine, pregabalin); podiatry care to prevent ulcers.
- Case 2 — Alcoholic Neuropathy (Toxic + Nutritional):
A 55-year-old man with long-standing alcohol excess presents with tingling and weakness in his legs. Exam: distal wasting, areflexia, sensory loss to vibration.
Diagnosis: Peripheral neuropathy due to alcohol toxicity and thiamine deficiency.
Management: Abstinence from alcohol, thiamine supplementation, physiotherapy.
- Case 3 — Vitamin B12 Deficiency (Nutritional):
A 45-year-old vegan develops progressive numbness in feet and unsteady gait. Exam: reduced vibration sense, positive Romberg, brisk reflexes (subacute combined degeneration).
Diagnosis: Peripheral neuropathy due to vitamin B12 deficiency.
Management: Parenteral vitamin B12 replacement; treat cause (e.g., pernicious anaemia).
- Case 4 — Charcot–Marie–Tooth Disease (Hereditary):
A 19-year-old man has progressive foot deformities and distal weakness. Exam: pes cavus, foot drop, absent ankle reflexes, glove-and-stocking sensory loss. Family history of similar symptoms.
Diagnosis: Hereditary motor and sensory neuropathy (Charcot–Marie–Tooth).
Management: Supportive: physiotherapy, orthotics, genetic counselling.
- Case 5 — Guillain–Barré Syndrome (Immune-Mediated, Acute):
A 33-year-old man develops ascending weakness 2 weeks after a diarrhoeal illness. Exam: areflexia, bilateral foot drop, and distal paraesthesia.
Diagnosis: Acute inflammatory demyelinating polyneuropathy (GBS).
Management: Admit for monitoring; IV immunoglobulin or plasma exchange; respiratory support if vital capacity drops.
Teaching Commentary 🧠
Peripheral neuropathies can be classified by pattern (sensory, motor, sensorimotor), time course (acute vs chronic), and cause (metabolic, toxic, nutritional, hereditary, immune, infectious).
- Diabetes = most common cause worldwide.
- Alcohol + nutritional deficiencies common in Western settings.
- Vitamin B12 deficiency gives mixed neuropathy + myelopathy.
- Charcot–Marie–Tooth = hereditary with pes cavus.
- GBS/CIDP = acute or chronic demyelinating immune neuropathies.
Approach: history, examination (distribution, symmetry, reflexes), then confirm with nerve conduction studies, bloods, and targeted tests. Management is always cause-specific + supportive.