| Download the app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. |
Transient Global Amnesia (TGA)
Introduction
- Transient Global Amnesia (TGA) is a short-lived, dramatic but ultimately benign episode of memory loss. The person suddenly can’t lay down new memories for a few hours, then goes back to normal.
- 📜 First properly described by Fisher & Adams in 1964.
- 🧠 The key picture: abrupt onset of anterograde amnesia and confusion about recent events, while the person still knows who they are, where they are, and their distant past.
- ❓ The exact cause is still debated – ideas include transient venous congestion, a migraine-like mechanism, brief hippocampal ischaemia, or stress-related vulnerability.
- ⚠️ It is easily mistaken for TIA or a seizure in the ED, but unlike those, the prognosis is excellent and most patients never have another episode.
📊 Epidemiology
- Incidence: roughly 5–10 cases per 100,000 people per year – so not common, but not ultra-rare either.
- 👵 Typically affects people in their 50s to 70s; it’s very unusual in young adults.
- 👨 There’s a slight male predominance in most series.
- 🔁 Recurrence happens in about 5–25% of patients, and if it does come back it’s usually just a single repeat episode many years later.
⚙️ Etiology & Pathophysiology
- 💧 One popular theory is transient venous congestion in the hippocampal region, leading to temporary dysfunction of memory circuits.
- ⚡ There are strong links with migraine in some patients, so a migrainous aura–type mechanism may play a role.
- 🩸 Some studies suggest brief hippocampal hypoperfusion, but not the sort of clear arterial occlusion you see in stroke.
- ⚡ Epileptic activity is thought to be unlikely in classic TGA – EEG is usually normal and there are no typical seizure features.
- ⏱️ Common triggers: sudden immersion in cold water, intense exertion, emotional shock, sexual activity, and sometimes medical or interventional procedures – i.e. anything that gives a big physiological or emotional jolt.
🩺 Clinical Presentation
- Sudden onset of anterograde amnesia with the classic repetitive questioning (“Where am I?”, “What’s happening?”) every few minutes.
- ✅ The person knows who they are and usually recognises family; older memories are mostly intact.
- ✅ They are awake, alert and able to follow commands; there is no loss of consciousness.
- ✅ There are no focal neurological deficits on examination (normal power, speech, visual fields, etc.).
- ⏳ The episode typically lasts 1–24 hours (most often 4–6 hours) and then fades, with memory gradually returning.
- ⏮️ A patch of retrograde amnesia (hours to days before the event) is common and may never fully come back.
- Patients usually feel very anxious or distressed during the episode – they’re aware that something is wrong, even if they can’t remember exactly what.
✅ Diagnostic Criteria (Practical Version)
- Witnessed episode of abrupt anterograde amnesia (family or staff can describe it).
- Clear inability to form new memories during the attack (repeats the same questions).
- No clouding of consciousness, no loss of personal identity, and the patient is otherwise “with it”.
- No focal neurological signs and no features suggesting a seizure (jerking, tongue bite, post-ictal confusion, etc.).
- Symptoms resolve completely within 24 hours.
- No recent significant head trauma to explain the amnesia.
🧾 Differential Diagnosis (Thinking Clinically)
- 🧩 Transient Ischaemic Attack (TIA): often has focal deficits (weakness, aphasia, hemianopia). Isolated amnesia without any other focal sign is unusual for a pure TIA.
- ⚡ Epileptic amnesia: events are usually shorter (minutes), may have automatisms, impaired awareness, post-ictal confusion, and an abnormal EEG.
- 🧠 Psychogenic/dissociative amnesia: often involves disturbed or lost identity, patchy autobiographical memory, and a strong psychological context.
- 🤕 Head injury: clear trauma history, possible LOC, headache, vomiting, or other concussion features.
- 🍷 Wernicke–Korsakoff: thiamine deficiency in heavy alcohol use – chronic confusion, ataxia, nystagmus, and confabulation rather than a single clean TGA episode.
- 💊 Drug-induced amnesia: classically benzodiazepines and other sedatives; the history often reveals recent medication or procedure.
🧪 Investigations (When the Picture Isn’t Textbook)
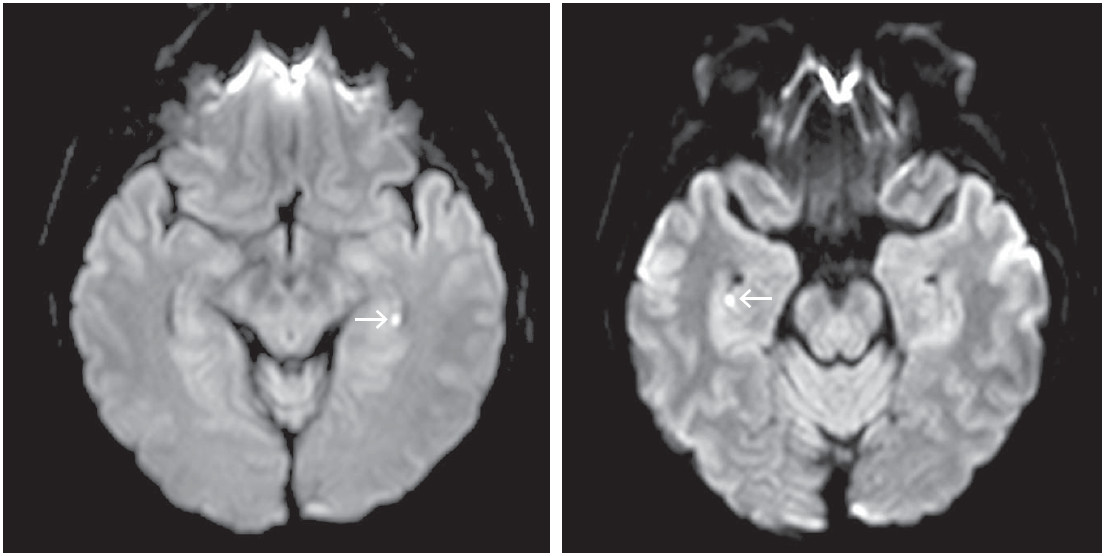
- 🧲 MRI with DWI: can show tiny punctate lesions in the hippocampus 24–48 hours after the event – supportive but not essential for diagnosis.
- 🖼️ CT head: usually normal; mainly used to rule out other acute pathology (e.g. bleed, large infarct) in the ED.
- 📉 EEG: typically normal in TGA; more useful if you’re genuinely worried about seizures.
- 🧪 Blood tests: check glucose, U&Es and other basics to rule out metabolic causes of confusion.
- 🫀 Cardiac / vascular work-up: ECG ± echo, carotid imaging if there are atypical features and TIA is still on the table.
💊 Management
- ✅ Reassurance is the main treatment. Explain that TGA looks frightening but is self-limiting and usually a one-off.
- 👀 Observe in a safe environment until the patient has clearly returned to baseline and you’re sure there is no stroke or seizure hiding underneath.
- 🚫 If the story and exam are classic, don’t automatically start anticoagulation or antiepileptic drugs – they don’t prevent TGA and add risk.
- 🧘 Explore and address obvious triggers (stress, sleep deprivation, acute emotional upset) and give simple advice on pacing and self-care.
- 🔁 Arrange follow-up, especially if the episode was atypical, prolonged, or if there is any diagnostic doubt.
📈 Prognosis
- 🌟 Prognosis is excellent – most people have a single episode and never see it again.
- 📉 Large cohort studies show no clear increase in stroke or epilepsy risk compared with the general population.
- 🧠 Cognitive function returns to normal, though there is often a “black hole” around the day of the event that never fully fills in.
- 🔁 Recurrence occurs in about 5–25% of patients, usually just once more over many years.
- 🚗 Driving (UK flavour): a single classic TGA episode doesn’t usually require DVLA notification; two or more documented episodes should prompt stopping driving and informing DVLA for individual assessment.
💡 Teaching Pearls
- 🗣️ In exams, the give-away phrase is “repetitive questioning in an otherwise well, alert patient” that lasts several hours.
- 🌊 Don’t forget common triggers like cold-water immersion, exertion, sexual activity or sudden emotional stress – examiners love that detail.
- ❌ Think pattern recognition:
- TGA → hours of pure anterograde amnesia, no focal signs, full recovery.
- TIA → focal deficit; isolated amnesia is unusual.
- Seizure → brief, stereotyped, with post-ictal phase.
- Psychogenic → identity disturbance and inconsistent exam.
- 👨⚕️ Your job at the bedside is to exclude dangerous mimics, then lean heavily into reassurance for the patient and family.
Conclusion
Transient Global Amnesia is a striking but ultimately self-limited amnestic syndrome: sudden onset, hours of repetitive questioning, then full recovery. If you recognise the pattern early, you can avoid over-treating it as stroke or epilepsy, minimise unnecessary investigations, and – most importantly – provide calm, confident reassurance to a very frightened patient and their relatives.
📚 References
- Hodges JR, Warlow CP. Syndromes of transient amnesia. J Neurol Neurosurg Psychiatry. 1990;53:834-843.
- Fisher CM, Adams RD. Transient global amnesia. Trans Am Neurol Assoc. 1964;89:143-147.
- Bartsch T, Deuschl G. TGA: functional anatomy and clinical implications. Lancet Neurol. 2010;9:205-214.
- Sattler JM, Rabinstein AA. Transient global amnesia. Mayo Clin Proc. 2019;94:662-672.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Disease
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
