| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Pulmonary Embolism 🫁
Related Subjects: |Pulmonary Embolism 🫁 |Assessing Breathlessness |Deep Vein Thrombosis |DVT/PE in pregnancy |CTPA In PE |Inferior Vena Cava Filter |Alteplase
🫁 Pulmonary emboli should be prevented by early mobilisation and low-dose LMWH in all at-risk patients. ⚠️ Untreated mortality is ~30%, which falls to ~8% with treatment.
| ⚕️ Stepwise Management of Suspected PE NICE NG158 aligned |
|---|
|
Pulmonary embolism is obstruction of the pulmonary arterial circulation, usually from thrombus arising in deep veins of the legs or pelvis. Untreated mortality approaches 25–30%, falling to <8% with anticoagulation. Early diagnosis, appropriate risk stratification, and prompt treatment are lifesaving.
🧬 Causes & Risk Factors (Virchow’s Triad)
- Venous stasis: immobility, long-haul travel, hospitalisation, paralysis, heart failure.
- Endothelial injury: surgery (especially orthopaedic), trauma, central venous lines.
- Hypercoagulability:
- Active cancer (pancreas, lung, gastric, brain, haematological highest risk).
- Pregnancy & postpartum (highest risk first 6 weeks postpartum).
- Oestrogen therapy (OCP, HRT).
- Inherited thrombophilia (Factor V Leiden, Prothrombin gene mutation, Protein C/S deficiency, Antithrombin deficiency).
- Antiphospholipid syndrome.
- Obesity, smoking.
- Other causes of embolic obstruction: fat embolism (fracture), amniotic fluid embolism, air embolism, tumour emboli (rare).
🧠 Pathophysiology
Acute embolic obstruction increases pulmonary vascular resistance, causing right ventricular (RV) pressure overload. The thin-walled RV dilates, impairing left ventricular preload and cardiac output. Hypoxaemia results from ventilation–perfusion mismatch and reduced mixed venous oxygen. Large PE may cause obstructive shock and sudden death.
🩺 Clinical Presentation
- Dyspnoea (most common).
- Pleuritic chest pain.
- Tachycardia, tachypnoea.
- Haemoptysis (infarction).
- Syncope or presyncope (suggests massive PE).
- Signs of DVT: unilateral leg swelling, calf tenderness.
- Massive PE: hypotension, raised JVP, loud P2, shock.
🧮 Diagnosis — Stepwise Approach (Adults, Non-Pregnant)
|
🫁 ASSESS WITH WELLS or GENEVA score
|
|---|
🧮 Wells and Geneva Score Components
In UK practice (NICE NG158), Wells score is most commonly used. Geneva may be useful where an entirely objective score is preferred.
| 🧮 Wells Score (UK NICE Preferred) | 📋 Revised Geneva Score (Objective) |
|---|---|
Score Components
Interpretation
|
Score Components
Interpretation
Geneva is fully objective and avoids clinician judgement bias. |
🧠 Practical Teaching Point
- Wells is NICE-recommended and most used in UK practice.
- Geneva is helpful when an entirely objective system is preferred.
- Haemodynamic instability overrides both — treat as massive PE immediately.
🔬 Investigations & Interpretation
- D-dimer: High sensitivity, low specificity. Elevated in infection, malignancy, pregnancy, elderly. Adjust normal expected levels to the patient age. Don't use in pregnancy is current advice. Some may find a normal dimer in pregnancy to be useful
- ABG: Type 1 respiratory failure (low O₂, low/normal CO₂).
- ECG: Sinus tachycardia most common. Possible RV strain (S1Q3T3, RBBB, T-wave inversion V1–V4).
- Troponin/BNP: Elevated in RV strain; prognostic marker.
- Chest X-ray: Often normal; may show effusion, wedge infarct. Can be done even if pregnant
- Doppler USS lower limb: Useful if pregnant and signs of DVT
- CTPA: First-line imaging; visualises intraluminal filling defects.
- V/Q scan: Useful in pregnancy or contrast allergy; mismatch suggests PE.
- Echocardiography: Reasonable if too unwell for CTPA to look for RV dilatation, septal flattening in massive/submassive PE to help judge need for Alteplase.
- Compression ultrasound: Proximal DVT → treat as PE equivalent.
Pulmonary artery anatomy
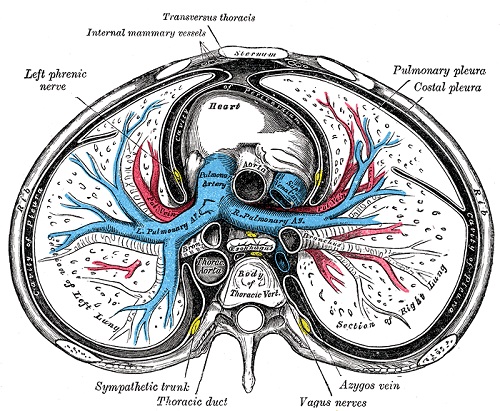
CT Pulmonary artery
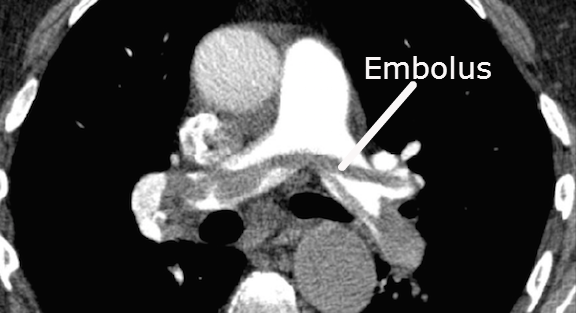
🖥️ CT Pulmonary Angiography (CTPA) |CTPA In PE
|
🫁 PE CONFIRMED: WHAT IS RISK OF DISCHARGE WITH PESI SCORE
|
|---|
⚡ Risk Stratification After Confirmation
- Massive (high-risk): SBP <90 mmHg or shock.
- Intermediate-risk: RV strain but normotensive.
- Low-risk: Haemodynamically stable, no RV strain.
- Use PESI or simplified PESI for prognostic assessment and outpatient suitability.
📊 Pulmonary Embolism Severity Index (PESI) & Simplified PESI
| 📋 Full PESI Score | 🩺 Simplified PESI (sPESI) |
|---|---|
Variables & Points
|
Variables (1 point each)
|
🧠 Teaching Pearls
- Wells / Geneva: Diagnostic tools (before imaging).
- PESI / sPESI: Prognostic tools (after PE confirmed).
- Haemodynamic instability overrides scoring systems — treat immediately.
- Outpatient PE management requires low PESI/sPESI, stable vitals, and good social support.
|
🫁 NOW CONTINUE TO TREAT CONFIRMED PE
|
|---|
💊 Management — General Principles
- Oxygen if hypoxic.
- Immediate therapeutic anticoagulation if PE suspected and imaging delayed.
- First-line anticoagulation: DOAC (Apixaban or Rivaroxaban).
- Apixaban 10 mg twice daily for 7 days. Then 5 mg twice daily. Extended prevention (after 6 months): 2.5 mg twice daily
- Rivaroxaban 15 mg twice daily for 21 days. Then 20 mg once daily. Extended prevention: 10 mg once daily (if low recurrence risk)
- Avoid DOACs in severe renal impairment (CrCl <15 mL/min), pregnancy, mechanical heart valves, and triple-positive antiphospholipid syndrome.
- Low Molecular Weight Heparin (LMWH)
- Preferred in pregnancy and sometimes in active cancer or high bleeding risk.
- Enoxaparin 1 mg/kg twice daily OR 1.5 mg/kg once daily (selected patients)
- Dalteparin 200 units/kg once daily (max 18,000 units daily) After 1 month: 150 units/kg once daily (cancer pathway)
- Reduce dose in renal impairment (CrCl <30 mL/min).
- Unfractionated Heparin (UFH)
- Use in severe renal impairment, high bleeding risk, or when rapid reversal may be needed (short half-life).
- IV bolus: 80 units/kg
- Then infusion: 18 units/kg/hour
- Adjust to APTT target (1.5–2.5× control)
- Warfarin
- Used if DOAC contraindicated (e.g., severe renal failure, antiphospholipid syndrome).
- Start 5 mg once daily (lower if elderly/frail)
- Overlap with LMWH for at least 5 days AND until INR 2–3 for 24 hours
- Target INR: 2.5 (range 2.0–3.0)
- Thrombolysis
- Large/Massive PE with Shock supported by CTPA or Echocardiogram ideally. RV dysfunction on echo, refractory hypoxia, raised troponin, extreme tachycardia, large clot burden, extreme tachycardia are all factors that might support alteplase. Take senior advice if unsure. Give Alteplase 10 mg IV bolus Then 90 mg over 2 hours (max total 100 mg) Indicated in PE with haemodynamic instability (SBP <90 mmHg or shock). The contraindication is any major bleeding risk - discuss with senior decision required. Cautious IV fluids (avoid RV overload). Vasopressors if shock. Consider catheter-directed therapy or surgical embolectomy if thrombolysis contraindicated or fails.
- Cardiac Arrest Suspected PE: Alteplase 50 mg IV bolus. Continue CPR for 60–90 minutes. Consider bedside echocardiography.
- Endovascular approach Talk to interventional radiology or cardiology whatever you might have locally if unable to use thrombolysis or failing to improve with thrombolysis
- ECMO may be considered for some cases. Discuss with ITU
- Duration of Treatmemt
- Provoked PE → 3 months treatment.
- Unprovoked PE → At least 3 months; consider extended therapy.
- Active cancer → DOAC preferred unless high bleeding risk.
- IVC filter only if anticoagulation contraindicated.
💊 Pulmonary Embolism (UK practice, NICE NG158 aligned)
Always check renal function, weight, bleeding risk, and drug interactions before prescribing. Doses below are standard adult doses — adjust in renal impairment, extremes of body weight, or frailty.
📌 Duration of Anticoagulation
- Provoked PE (surgery, transient risk factor) → 3 months
- Unprovoked PE → At least 3 months, reassess for extended therapy
- Recurrent PE → Long-term anticoagulation
- Cancer-associated → ≥6 months, often ongoing
🛑 Inferior Vena Cava (IVC) Filter
- Indication: Absolute contraindication to anticoagulation OR recurrent PE despite treatment
- Use retrievable filter where possible
- Remove once anticoagulation safe
🧠 Practical Prescribing Pearls
- Check renal function before DOAC or LMWH.
- Review weight — obesity may require dosing adjustment.
- Assess bleeding risk (HAS-BLED factors).
- Review interacting drugs (azoles, antiepileptics, rifampicin).
- Reassess need for anticoagulation at 3 months.
