| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Spinal and Epidural Anaesthesia
Related Subjects: | General Anaesthetics | Introduction to Anaesthetics | Spinal and Epidural Anaesthesia | Local Anaesthetics for Suturing or other Procedures | Post-operative Surgical Care and Complications | Rapid Sequence Intubation (RSI)
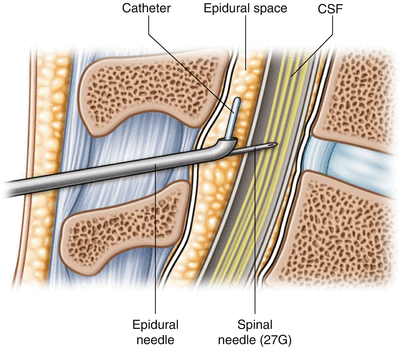
Spinal and epidural anaesthesia are both forms of regional anaesthesia that block pain by interrupting nerve transmission at the level of the spinal cord. Both techniques enable surgery or labour analgesia while maintaining consciousness. The key difference is that spinal anaesthesia delivers a single dose into the subarachnoid space (CSF), whereas epidural anaesthesia deposits the drug into the epidural space for titratable, prolonged action.
🧠 Relevant Anatomy
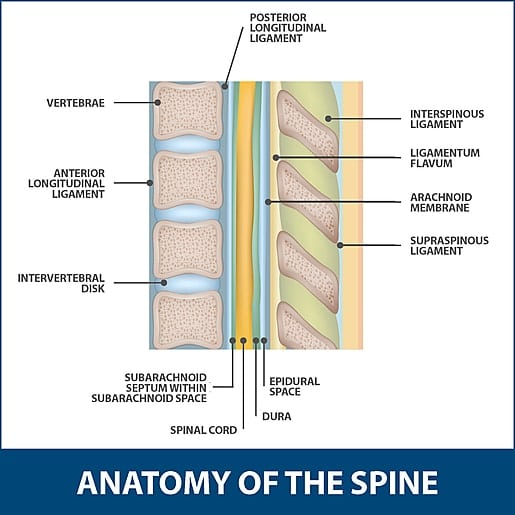
- The spinal cord extends from the foramen magnum to approximately L1–L2 in adults, continuing as the cauda equina.
- The spinal meninges comprise:
- Dura mater: Tough outer layer.
- Arachnoid mater: Thin middle layer enclosing the cerebrospinal fluid (CSF).
- Pia mater: Delicate layer adhering to the cord surface.
- Epidural space: Lies between the dura mater and the vertebral canal; contains fat, connective tissue, and venous plexuses (Batson’s plexus).
- Subarachnoid space: Lies between the arachnoid and pia mater; filled with CSF and communicates freely with the brain ventricles.
- In both techniques, the puncture is usually performed below L2 (L3/L4 or L4/L5) to avoid spinal cord injury — the landmark is the Tuffier’s line connecting the iliac crests.
💉 Spinal Anaesthesia
- Injection Site: Into the subarachnoid space through the dura and arachnoid mater.
- Onset and Duration: Rapid onset (1–3 minutes), duration typically 1–2 hours depending on the agent used (e.g. bupivacaine, lidocaine).
- Needle: Fine (25G–27G) pencil-point needles reduce post-dural puncture headache (PDPH).
- Effect: Produces a dense motor and sensory block; sympathetic block may cause hypotension and bradycardia.
- Distribution: Spread depends on dose, baricity, patient position, and CSF dynamics.
- Common Agents: Hyperbaric bupivacaine, lidocaine (shorter acting), sometimes with opioids (fentanyl, morphine) for enhanced analgesia.
- Complications:
- Hypotension (sympathetic blockade).
- Bradycardia (unopposed vagal tone).
- Post-dural puncture headache.
- High or total spinal block if excessive spread occurs → respiratory compromise.
- Uses: Ideal for lower abdominal, pelvic, and lower limb surgery (e.g. hernia repair, C-section, orthopaedic procedures).
🧬 Epidural Anaesthesia
- Injection Site: Into the epidural space outside the dura mater — typically at the lumbar or thoracic level.
- Technique: A larger Tuohy needle is used to introduce a fine catheter (18G–20G). Loss-of-resistance (saline or air) technique identifies the space.
- Onset and Duration: Slower (10–20 minutes). Duration is adjustable by continuous infusion or bolus dosing through the catheter.
- Effect: Segmental and titratable block — predominantly sensory with variable motor involvement.
- Common Agents: Bupivacaine, ropivacaine, levobupivacaine; often combined with opioids for synergistic analgesia.
- Advantages:
- Adjustable depth and extent of block.
- Prolonged analgesia (e.g. labour, postoperative pain control).
- Less risk of profound hypotension compared to spinal.
- Complications:
- Accidental dural puncture (→ PDPH if not recognised).
- Hypotension (sympathetic block).
- Epidural haematoma or abscess (rare).
- Local anaesthetic systemic toxicity (LAST) if intravascular injection occurs.
- Uses: Obstetric analgesia, major abdominal/thoracic surgery (as thoracic epidural), and chronic pain management.
⚖️ Comparison Table
| Feature | Spinal Anaesthesia | Epidural Anaesthesia |
|---|---|---|
| Site of injection | Subarachnoid space (CSF) | Epidural space (outside dura) |
| Needle | Fine 25–27G | Larger Tuohy 18–20G |
| Catheter | Single injection only | Catheter for continuous infusion |
| Onset | 1–3 min (rapid) | 10–20 min (slower) |
| Duration | 1–2 hours | Variable (hours–days) |
| Block | Total block below level; motor + sensory | Segmental; mainly sensory |
| Control | Fixed dose | Titratable and adjustable |
| Hypotension risk | Common | Less pronounced |
| Main uses | Caesarean section, lower limb surgery | Labour, thoracic/abdominal analgesia |
🩺 Physiological Effects
- Cardiovascular: Sympathetic blockade causes vasodilation → ↓ venous return and BP. High spinal may affect cardiac accelerator fibres (T1–T4).
- Respiratory: Minimal in lower blocks; high blocks may impair intercostal muscle function.
- Gastrointestinal and urinary: Parasympathetic predominance → increased gut motility; urinary retention may occur post-procedure.
- Thermoregulation: Vasodilation and reduced shivering thresholds contribute to hypothermia.
🧠 Clinical Pearls
- Perform under strict aseptic technique with continuous monitoring (ECG, BP, SpO₂).
- Always check for aspiration of CSF in spinal and absence of CSF or blood in epidural placement.
- Use test doses in epidural to detect intrathecal or intravascular injection (e.g. 3 mL lidocaine + adrenaline).
- Preload with IV fluids before spinal to reduce hypotension risk.
- Document block level (loss of sensation to cold or pinprick).
🧪 Pharmacology Context
- Common local anaesthetics:
- Lidocaine: Rapid onset, short duration (used less for spinal due to transient neurological symptoms).
- Bupivacaine: Long-acting, high potency; potential for cardiac toxicity if misinjected IV.
- Ropivacaine/Levobupivacaine: Similar efficacy but safer cardiovascular profile.
- Adjuvants: Opioids (fentanyl, morphine), clonidine, or dexmedetomidine enhance analgesia and prolong block.
📷 Visual Summary
💡 Teaching Tip: Think of spinal anaesthesia as a “single-shot lightning strike” — fast, intense, complete — and epidural as a “slow-burning candle” — controllable, extendable, and gentle. Both rely on blocking sodium channels in nerve fibres to interrupt conduction, but differ in depth, spread, and flexibility. Mastering their anatomy and physiology is essential for safe regional anaesthetic practice.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
