| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
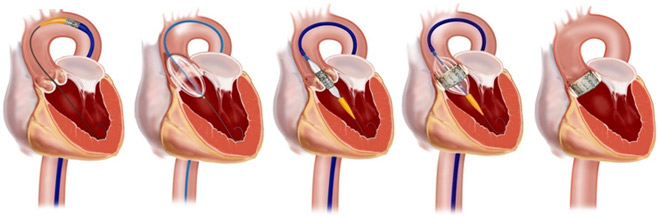
Transcatheter aortic valve implantation/replacement (TAVI/R)
Related Subjects: |Aortic Anatomy |Acute Coronary Syndrome (ACS) General |Aortic Dissection |Acute Heart Failure and Pulmonary Oedema |Aortic Regurgitation (Incompetence) |Aortic Stenosis |Aortic Sclerosis |Transcatheter aortic valve implantation (TAVI)
🫀 TAVI is a catheter-based aortic valve replacement (usually transfemoral) that avoids sternotomy and cardiopulmonary bypass.
📌 Randomised data in inoperable severe aortic stenosis (PARTNER cohort B) showed TAVI is superior to medical/standard therapy with durable benefit to 5 years.
📘 About
- 🕰️ First-in-human TAVI was performed in 2002 (Cribier; “last resort” in critical AS).
- 👵 Commonly considered in older adults; modern practice spans a wide risk range (low–high) depending on age, anatomy, frailty, and surgical risk.
- 🧠 Core principle: decision made by a Heart Team / TAVI MDT (cardiology + cardiac surgery + imaging + anaesthetics + geriatrics where relevant).
- 🏥 UK outcomes are tracked via the national TAVI registry (NICOR).
✅ Who is considered for TAVI? (Practical criteria)
- Severe aortic stenosis AND symptoms (exertional dyspnoea, angina, syncope/presyncope, HF/pulmonary oedema), or objective evidence of decompensation.
- Severity typically supported by echo: e.g. valve area ≤1.0 cm2, mean gradient ≥40 mmHg, or Vmax ≥4.0 m/s (with attention to low-flow/low-gradient phenotypes).
- Heart Team factors:
- 🧓 Age (TAVI often favoured ≥75, but individualised).
- 🧱 Surgical risk (STS/EuroSCORE II), but also “non-score” risks: frailty, porcelain aorta, prior chest radiotherapy, hostile chest, severe lung disease.
- 🧬 Anatomy: annulus size, LVOT/calcification pattern, coronary heights, aortic root geometry, bicuspid valve considerations.
- 🦵 Access feasibility (transfemoral preferred): femoral/iliac calibre & tortuosity, calcification, aortic atheroma.
- 🧑⚕️ In the UK, “turned down for surgery” is no longer the only pathway—many centres offer TAVI to patients who are technically operable but best served by a transcatheter approach after MDT review.
🚫 When TAVI may be unsuitable (examples)
- Active infection/endocarditis or sepsis (delay until treated).
- Annulus/access anatomy not suitable for safe valve delivery/anchoring.
- Life expectancy limited by non-cardiac disease where valve intervention won’t improve symptoms/quality of life (MDT + patient goals matter).
⚠️ Complications (typical contemporary ranges — vary by valve type, risk profile, and centre)
- ☠️ 30-day mortality: ~1–3% (higher in very frail/high-risk cohorts).
- 🧠 Stroke: ~2–3% (peri-procedural + early post-op).
- 🦵 Major vascular complications: ~3–6% (access-site bleeding/dissection/closure failure).
- 💓 Conduction disturbance → permanent pacemaker: commonly ~8–15% (can be higher with self-expanding valves / baseline RBBB).
- 🌊 Paravalvular leak (PVL): usually mild; moderate–severe PVL is now uncommon but clinically important.
- 🩸 Bleeding, AKI, coronary obstruction (rare but catastrophic), tamponade, annular/aortic root rupture (<1% in most series).
🛠️ Procedure (what usually happens)
- 🧭 Pre-op work-up usually includes:
- CT aortogram “TAVI protocol” (annulus sizing + coronary heights + access mapping).
- Coronary assessment (CTCA or invasive angiography; PCI selectively if indicated).
- Echo (severity, LV function, valve morphology) + frailty/functional assessment.
- 🦵 Transfemoral is the commonest route (alternatives: subclavian/axillary, carotid, transcaval, transapical in selected centres).
- 💤 Many transfemoral cases are performed under local anaesthetic ± conscious sedation; GA reserved for selected cases (airway, complexity, instability).
- 🧷 Temporary pacing is often used during deployment; anticoagulation during the case is typically with IV heparin (per protocol).
- 🧫 Antibiotic prophylaxis is given pre-procedure, but the exact regimen varies by centre—use your local cath-lab/TAVI pathway.
🏥 Post-op (high-yield ward points)
- 📈 Continuous ECG monitoring: watch for new LBBB, PR prolongation, or high-grade AV block (risk highest early).
- 🫀 Echo: often immediately post-procedure and/or pre-discharge to assess gradients, PVL, LV function, and complications.
- 🧑⚕️ Follow-up commonly at 6–8 weeks, then periodically (often annually) in valve clinic.
💊 Antithrombotics after TAVI (modern “minimalist” approach)
- No indication for oral anticoagulation (OAC): usually single antiplatelet therapy (often aspirin 75 mg daily) rather than routine DAPT.
- Indication for OAC (e.g. AF): usually OAC alone (avoid adding antiplatelet unless there is another clear reason such as recent stent).
- DAPT (aspirin + clopidogrel) is generally reserved for patients with a recent coronary stent/ACS and should be time-limited with bleeding risk in mind.
🧾 References
- Kapadia SR et al. 5-year outcomes of TAVR vs standard therapy in inoperable severe AS (PARTNER cohort B). The Lancet, 2015.
- POPular TAVI Trial (aspirin alone vs aspirin + clopidogrel post-TAVI in patients without OAC indication). NEJM, 2020.
- ESC/EACTS Valvular Heart Disease Guidelines (latest update). ESC, 2025.
- NICE IPG586: Transcatheter aortic valve implantation for aortic stenosis (interventional procedures guidance).
- NICOR: National TAVI programme / registry (UK outcomes reporting).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
