| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Heterochromia Iridium
👁️ Heterochromia — a difference in iris colour between the two eyes or within one eye. Usually benign, but occasionally a sign of underlying systemic or ocular disease. ⚠️ Neuroblastoma (childhood) and melanoma (later life, with dark iris spot) are rare but important causes of acquired heterochromia.
🌈 About
- Heterochromia means different eye colours or multi-toned irises within one eye.
- Usually harmless and may be congenital or acquired.
- Common in animals (e.g. huskies, cats), rare in humans.
🧬 Types
- 🔹 Complete heterochromia: Each eye a different colour (e.g., one blue, one brown).
- 🔸 Sectoral / partial heterochromia: Segment of one iris differs in colour (as below).
- 🔹 Central heterochromia: Inner ring around pupil differs from outer iris colour.
🎨 Split Iris (Sectoral Heterochromia)

Example of partial heterochromia — a wedge of lighter pigment within one iris.
👶 Heterochromia in Infancy — Causes
- 🌈 Benign (physiological) heterochromia — normal pigment variation.
- 🦋 Horner’s syndrome (congenital) — smaller pupil (miosis), mild ptosis, lighter iris.
- 🧠 Sturge–Weber syndrome — facial port-wine stain, glaucoma risk.
- 🎧 Waardenburg syndrome — white forelock, broad nasal root, deafness.
- 🧬 Piebaldism — patchy albinism of skin and hair.
- 🚼 Hirschsprung disease — may co-occur in syndromic forms (e.g., Waardenburg type IV).
- 🌀 Bloch–Sulzberger syndrome (Incontinentia pigmenti).
- 📘 Neurofibromatosis (von Recklinghausen disease).
- 🍃 Tuberous sclerosis (Bourneville disease).
- 🕊️ Parry–Romberg syndrome — facial hemiatrophy, sometimes with iris pigment loss.
🧑⚕️ Waardenburg Syndrome (example)
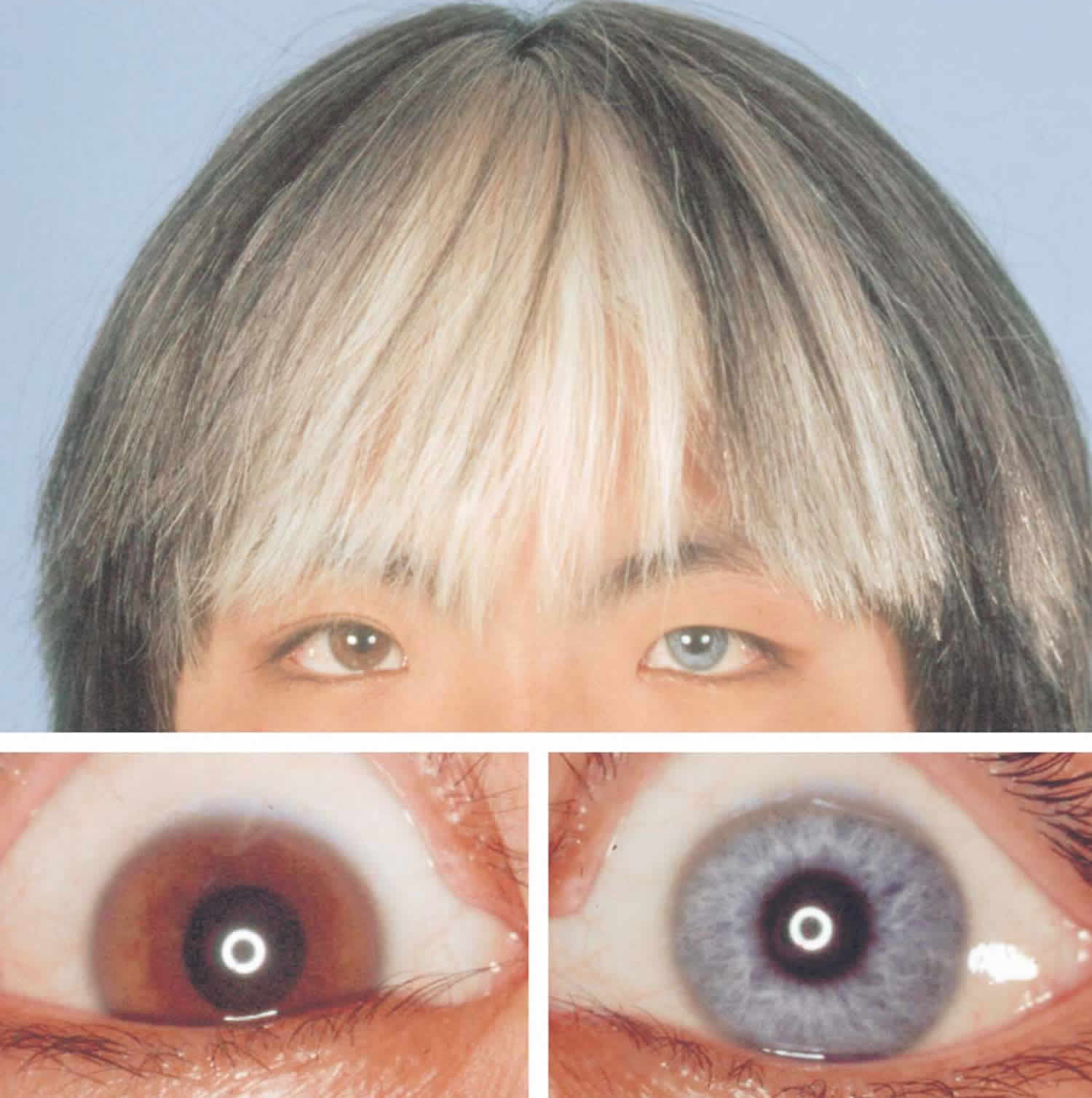
Note iris colour variation, white forelock, and characteristic facial features.
⚡ Acquired Heterochromia — Causes
- 🩸 Eye trauma or post-surgical pigment change.
- 🧠 Neuroblastoma (childhood) — tumour of sympathetic chain; may present with unilateral Horner’s syndrome.
- 🦠 Inflammation: Iritis, uveitis, Fuchs’ heterochromic cyclitis.
- 💊 Medications: Prostaglandin analogues for glaucoma (e.g., latanoprost, bimatoprost, “Latisse”).
- 🌀 Glaucoma or pigment dispersion syndrome.
- 🎯 Melanoma or melanocytoma of the iris — often darkened, irregular patch.
- 💉 Bleeding (hyphema) or iron deposition post-injury.
- 🧩 Horner’s syndrome (acquired) — lighter iris on affected side.
- 💧 Posner–Schlossman syndrome — recurrent uveitic glaucoma.
- 🧬 Chediak–Higashi syndrome — albinism, immune defects.
- ⚡ Diabetes / CRVO — rare secondary pigment changes.
🩺 Clinical Evaluation
- Assess onset, laterality, visual acuity, photophobia, pain.
- Look for pupil asymmetry, eyelid ptosis (Horner’s), or signs of uveitis/glaucoma.
- Use slit-lamp examination to confirm iris pigment change (not reflection or shadow).
🧭 Management
- 👶 At birth: Discuss with paediatrician; often benign pigment development, but consider ophthalmology referral.
- 🧑⚕️ Later in life: Refer to ophthalmologist if new or changing heterochromia to exclude melanoma or uveitis.
- ⚕️ Treat underlying cause if identified (infection, inflammation, or trauma).
- 📸 Baseline photograph — useful for monitoring progression.
💡 Teaching tip: - Congenital = likely benign (esp. stable since infancy). - Acquired = always investigate (rule out tumour, inflammation, or trauma). - Horner’s syndrome can be recognised by triad: ptosis + miosis + anhidrosis ± lighter iris.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
