| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Bile salt malabsorption (BAM)
Bile salt malabsorption (BAM) is a condition where excess bile salts reach the colon due to defective ileal absorption or inappropriate hepatic secretion. This causes stimulation of colonic fluid and electrolyte secretion, resulting in chronic watery diarrhoea. 🚽
📖 About
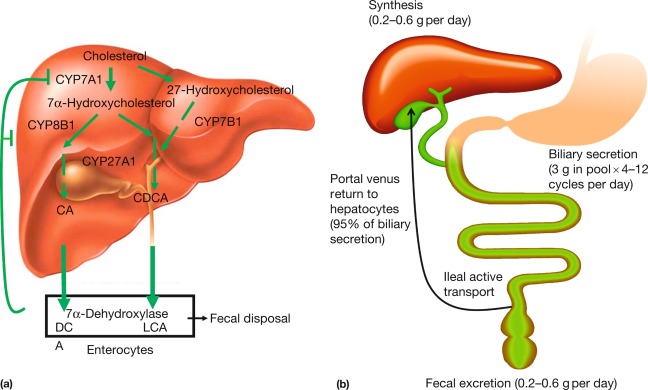
- Bile salts are synthesised in the liver from cholesterol and play a key role in fat digestion and absorption.
- Normally, 95% are reabsorbed in the terminal ileum and recycled via the enterohepatic circulation 🔄.
- In BAM, this recycling is disrupted → excess bile acids spill into the colon → irritation, secretion, and rapid transit.
🧬 Aetiology (Types of BAM)
- Type 1: Secondary to ileal disease or resection (e.g., Crohn’s ileitis, terminal ileal resection).
- Type 2: Primary/idiopathic BAM with no obvious structural abnormality.
- Type 3: Secondary to other GI disorders (e.g., coeliac disease, chronic pancreatitis, post-cholecystectomy, SIBO).
🩺 Clinical Features
- Chronic watery diarrhoea 💧 (often mistaken for IBS-D).
- Urgency and faecal incontinence.
- Bloating and abdominal cramps.
- Steatorrhoea and fat-soluble vitamin deficiencies (in severe cases).
- History of ileal disease, surgery, or gallbladder removal often present.
🔬 Investigations
- SeHCAT test (75Se-homotaurocholic acid test): Nuclear medicine scan; <10% retention at 7 days = BAM. 📉
- Serum C4 (7α-hydroxy-4-cholesten-3-one): Marker of bile acid synthesis (raised in BAM).
- Faecal bile acid measurement: Detects excess bile acids in stool.
- Routine bloods to exclude other causes: FBC, CRP, coeliac screen, thyroid function.
⚕️ Management
- Bile acid sequestrants (first-line):
- Cholestyramine 🥤 (powdered resin) — effective but poorly tolerated (bloating, flatulence, poor palatability).
- Colesevelam 💊 — better tolerated tablet form, though more expensive.
- Dietary advice: Low-fat diet may reduce symptoms.
- Vitamin supplementation: Fat-soluble vitamins (A, D, E, K) if deficiencies are present.
- Treat underlying cause: e.g., Crohn’s therapy, coeliac gluten-free diet.
📊 Prognosis
- BAM is often underdiagnosed; up to 30% of patients with “IBS-D” may actually have BAM.
- Most patients respond well to bile acid sequestrants, though adherence can be limited by tolerability.
- Untreated BAM → chronic diarrhoea, impaired quality of life, malnutrition.
📚 References
🌿 Introduction
Bile salt malabsorption (BAM) is a condition where excess bile salts reach the colon due to defective ileal absorption or inappropriate hepatic secretion. This causes stimulation of colonic fluid and electrolyte secretion, resulting in chronic watery diarrhoea. 🚽
📖 About
- Bile salts are synthesised in the liver from cholesterol and play a key role in fat digestion and absorption.
- Normally, 95% are reabsorbed in the terminal ileum and recycled via the enterohepatic circulation 🔄.
- In BAM, this recycling is disrupted → excess bile acids spill into the colon → irritation, secretion, and rapid transit.
🧬 Aetiology (Types of BAM)
- Type 1: Secondary to ileal disease or resection (e.g., Crohn’s ileitis, terminal ileal resection).
- Type 2: Primary/idiopathic BAM with no obvious structural abnormality.
- Type 3: Secondary to other GI disorders (e.g., coeliac disease, chronic pancreatitis, post-cholecystectomy, SIBO).
🩺 Clinical Features
- Chronic watery diarrhoea 💧 (often mistaken for IBS-D).
- Urgency and faecal incontinence.
- Bloating and abdominal cramps.
- Steatorrhoea and fat-soluble vitamin deficiencies (in severe cases).
- History of ileal disease, surgery, or gallbladder removal often present.
🔬 Investigations
- SeHCAT test (75Se-homotaurocholic acid test): Nuclear medicine scan; <10% retention at 7 days = BAM. 📉
- Serum C4 (7α-hydroxy-4-cholesten-3-one): Marker of bile acid synthesis (raised in BAM).
- Faecal bile acid measurement: Detects excess bile acids in stool.
- Routine bloods to exclude other causes: FBC, CRP, coeliac screen, thyroid function.
⚕️ Management
- Bile acid sequestrants (first-line):
- Cholestyramine 🥤 (powdered resin) — effective but poorly tolerated (bloating, flatulence, poor palatability).
- Colesevelam 💊 — better tolerated tablet form, though more expensive.
- Dietary advice: Low-fat diet may reduce symptoms.
- Vitamin supplementation: Fat-soluble vitamins (A, D, E, K) if deficiencies are present.
- Treat underlying cause: e.g., Crohn’s therapy, coeliac gluten-free diet.
📊 Prognosis
- BAM is often underdiagnosed; up to 30% of patients with “IBS-D” may actually have BAM.
- Most patients respond well to bile acid sequestrants, though adherence can be limited by tolerability.
- Untreated BAM → chronic diarrhoea, impaired quality of life, malnutrition.
📚 Cases — Bile Salt Malabsorption
- Case 1 (Crohn’s-related BAM): 👩🦳 A 38-year-old woman with a history of Crohn’s ileitis (post-ileal resection) presents with chronic watery diarrhoea, urgency, and bloating. Symptoms were initially misdiagnosed as “IBS.” A SeHCAT test shows <5% retention at 7 days. Management: Started on colesevelam and low-fat diet. Outcome: Marked improvement in stool frequency and urgency. Maintains symptom control with long-term bile acid sequestrant.
- Case 2 (Idiopathic BAM mislabelled as IBS): 👨🦱 A 45-year-old man reports 2 years of postprandial watery diarrhoea and bloating. Previous work-up (bloods, coeliac screen, colonoscopy) was normal. Initially treated as IBS-D without success. SeHCAT retention is 7%. Management: Started on cholestyramine powder, titrated gradually, plus dietary counselling. Outcome: Dramatic improvement in symptoms; able to return to work after years of disrupted quality of life.
🧑⚕️ Teaching Commentary
Bile salt malabsorption is a frequent but under-recognised cause of chronic diarrhoea. It should be suspected in patients labelled with IBS-D, especially with a history of ileal resection, cholecystectomy, or Crohn’s disease. 🔑 SeHCAT is the UK gold standard for diagnosis, but empirical trials with bile acid sequestrants can also be useful. Effective treatment transforms quality of life.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
