| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Achalasia
Related Subjects: |Achalasia |American Trypanosomiasis (Chagas Disease) |Oesophageal Carcinoma |Diffuse Oesophageal spasm |Diffuse Oesophageal Perforation - Rupture |Gastro-Oesophageal Reflux
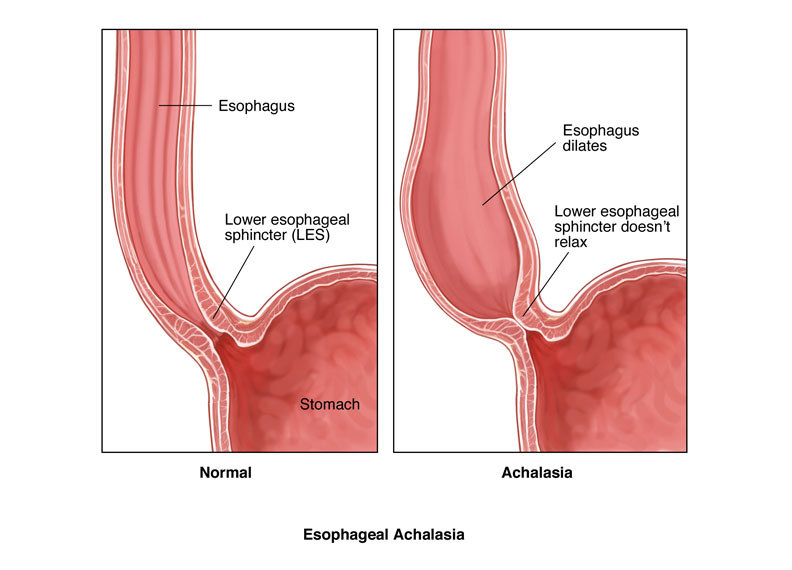
🥤 Achalasia is a chronic oesophageal motility disorder caused by degeneration of ganglion cells in the myenteric plexus. This leads to failure of the lower oesophageal sphincter (LES) to relax, impaired peristalsis, and progressive dysphagia. ⚠️ In older patients, always rule out oesophageal cancer first.
📌 About
- Primary oesophageal motility disorder with progressive difficulty swallowing both solids and liquids.
- “Achalasia” derives from Greek = “fails to relax.”
- Functional obstruction occurs due to persistent LES contraction.
📊 Epidemiology
- Most common between 30–60 years but can present at any age.
- Incidence ≈ 1 in 100,000 per year.
🧬 Aetiology & Pathophysiology
- Failure of LES relaxation → impaired food passage.
- Loss of ganglion cells in myenteric plexus + reduced nitric oxide & VIP synthesis.
- Degeneration of vagal input also contributes.
- Mimics Chagas disease in endemic South America (Trypanosoma cruzi).
🤒 Clinical Features
- Progressive dysphagia to solids & liquids (contrast with cancer = solids first).
- Regurgitation of undigested food, nocturnal coughing, aspiration.
- Inability to belch → bloating & chest discomfort.
- Chest pain, weight loss, hiccups, reflux-like symptoms.
- Many patients adapt by drinking water with meals or performing Valsalva-like manoeuvres.
🔎 Investigations
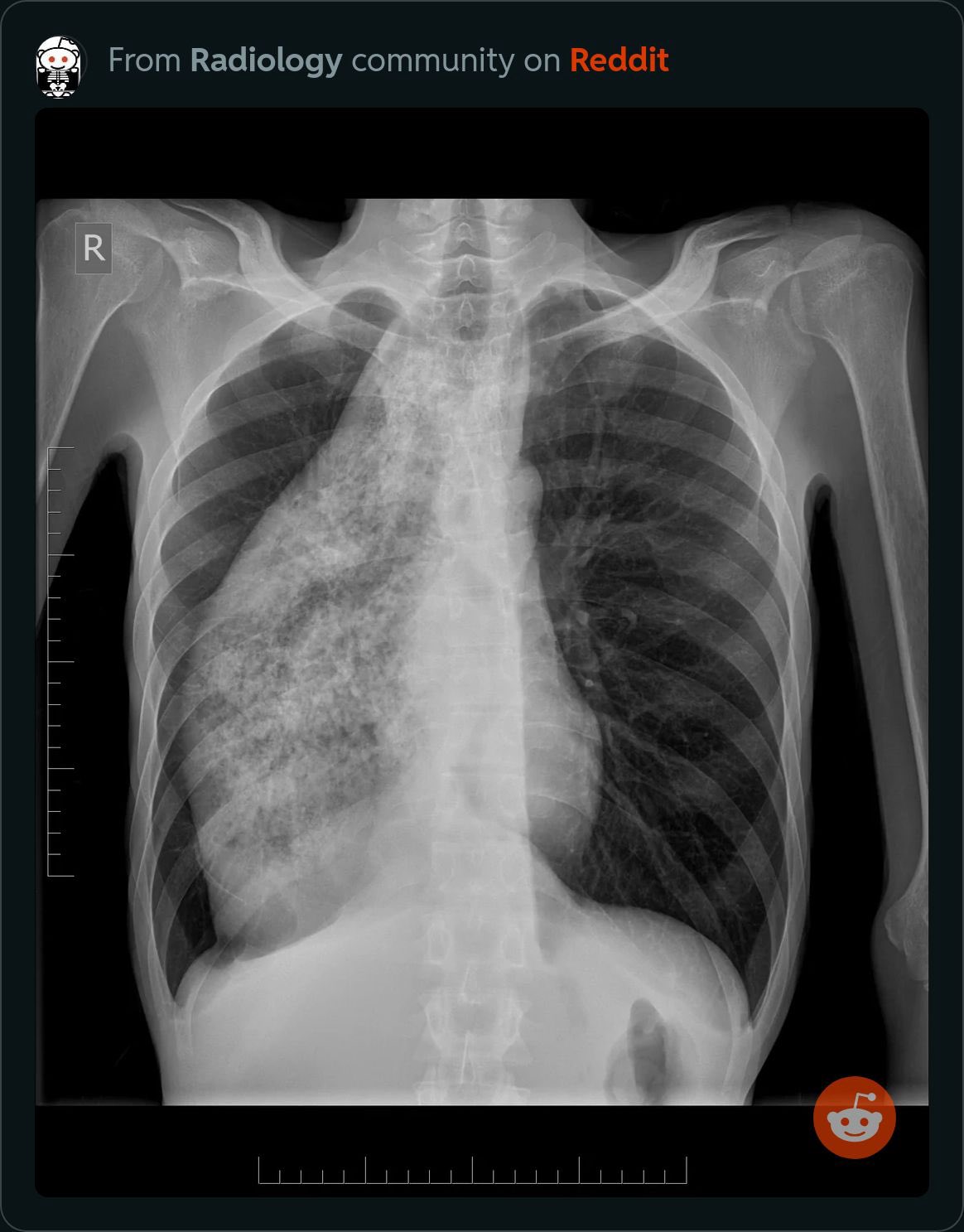
- CXR: May show wide, fluid-filled oesophagus, absent fundal gas, aspiration changes.
- Barium swallow: Classic “bird’s beak” tapering at LES with proximal dilation.
- Oesophageal manometry (gold standard): High LES pressure (>45 mmHg), incomplete relaxation, absent distal peristalsis.
- Endoscopy: To exclude malignancy/stricture.
- Serology: T. cruzi testing if relevant travel history (rule out Chagas).
- Bloods: FBC, U&E, LFT, glucose – assess comorbidity & complications.
🧾 Differentials
- Oesophageal cancer: Dysphagia starts with solids → later liquids.
- Oesophageal stricture: Benign (GERD) or malignant.
- Chagas disease: In endemic regions; identical physiology.
💊 Management
- Medical: CCBs (nifedipine), nitrates (GTN) → lower LES tone; limited by side effects.
- Botulinum toxin injection: 85% response but temporary (requires repeat).
- Pneumatic balloon dilation: Widens LES, risk of perforation.
- Surgery (Heller’s myotomy): Minimally invasive; often combined with fundoplication to prevent reflux.
- Lifestyle & reflux control: Small meals, eat slowly, water with meals, head-of-bed elevation, avoid late meals.
- Cancer surveillance: Long-standing achalasia ↑ risk of oesophageal SCC.
⚠️ Complications
- 🌙 Aspiration pneumonia (especially nocturnal regurgitation).
- ⬆️ 15x risk of oesophageal squamous carcinoma.
- 💀 Malnutrition & weight loss.
📚 References
Cases — Achalasia
- Case 1: A 35-year-old man presents with 12 months of progressive dysphagia to both solids and liquids, regurgitation of undigested food at night, and 5 kg weight loss. He reports occasional chest discomfort after meals. Barium swallow shows a “bird’s beak” tapering of the distal oesophagus. Oesophageal manometry confirms absent peristalsis and incomplete relaxation of the lower oesophageal sphincter (LOS).
Management: Endoscopic pneumatic dilatation of the LOS performed, with advice on small frequent meals and head-up sleeping.
Outcome: Symptoms improve significantly, weight stabilises, and he remains under annual review for recurrence and malignancy risk. - Case 2: A 62-year-old woman presents with long-standing dysphagia and recurrent aspiration pneumonias. She describes nocturnal coughing and post-prandial regurgitation. She is cachectic (BMI 17). CT chest excludes malignancy; manometry shows type II achalasia.
Management: Laparoscopic Heller’s myotomy with partial fundoplication undertaken after nutritional optimisation. Peri-operative antibiotics given for aspiration pneumonia risk.
Outcome: Excellent resolution of dysphagia, improved nutritional status at 6 months, and no further aspiration episodes.
Teaching Commentary 🧑⚕️
Achalasia results from loss of inhibitory ganglion cells in the oesophageal myenteric plexus, leading to absent peristalsis and failure of LOS relaxation. Symptoms include dysphagia (solids + liquids), regurgitation, chest pain, and weight loss. Diagnosis is with oesophageal manometry, supported by barium swallow. Management options: • Pneumatic dilatation (less invasive, risk of perforation). • Heller’s myotomy ± fundoplication (durable surgical option). • Botulinum toxin injection (palliative/elderly/unfit). Patients remain at higher risk of oesophageal squamous carcinoma, so long-term surveillance is important.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
