| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Macrophage activation syndrome (MAS)
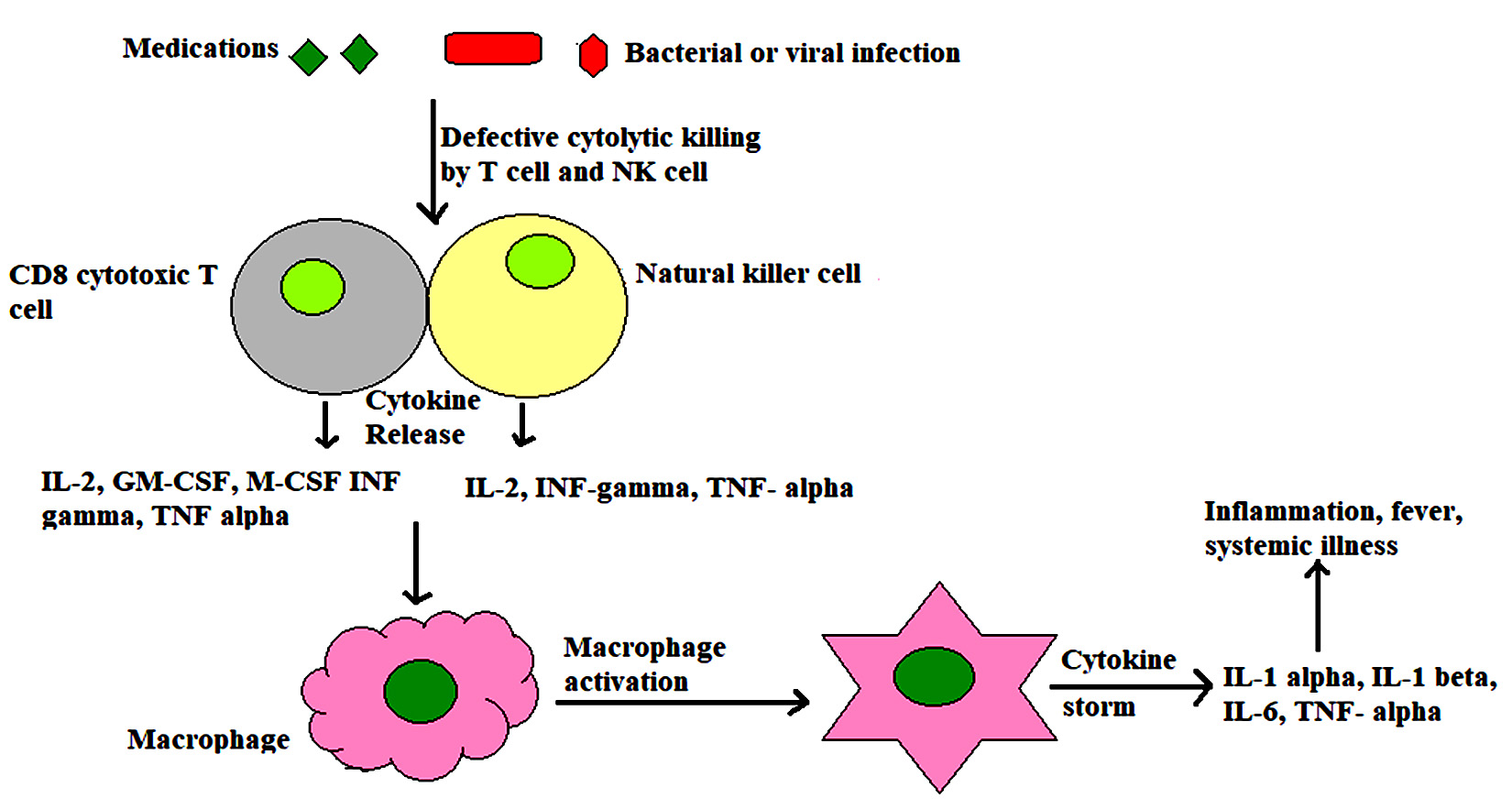
What it is: MAS is a life-threatening hyperinflammatory state on the spectrum of secondary HLH, most often complicating systemic JIA / adult-onset Still’s, but also SLE, vasculitis, infection, or malignancy. A failure of cytotoxic (NK/CTL) pathways → unchecked macrophage activation → a cytokine storm (💥 IL-1, IL-6, IFN-γ) causing fever, cytopenias, hepatitis, coagulopathy, and multi-organ failure.
🚨 When to suspect it (red flags)
- 🧯 Unremitting fever in known Still’s/sJIA/SLE, “septic but cultures negative.”
- 📉 Platelets fall; ESR falls while CRP and ferritin rise.
- 🧪 Very high ferritin (often >3,000 µg/L; may be >10,000). Trend > single value.
- 🩸 Coagulopathy (↓fibrinogen), ↑triglycerides, ↑LDH, transaminitis, hyponatraemia, ± hepatosplenomegaly.
- ⚠️ Deterioration despite “usual” therapy (CRP can be blunted on tocilizumab).
🔍 Key differentials
- 🦠 Sepsis (may coexist) — treat empirically while evaluating.
- 🔥 Underlying disease flare without MAS.
- 🧫 Other sHLH (malignancy/infection-associated), TTP/HUS, acute liver failure.
🧪 Initial investigations (STAT + daily trends)
- 🧾 FBC (cytopenias), coagulation (PT/APTT, fibrinogen, D-dimer), U&Es, LFTs, CRP, ESR, ferritin, triglycerides, LDH.
- 🧫 Blood/urine cultures, CXR; targeted viral PCRs (EBV/CMV/resp) as indicated; source imaging.
- 🖥️ Abdo US (organomegaly); echo if shock/myopericarditis.
- 🧬 Consider sCD25 (soluble IL-2R) / NK activity if available. Bone marrow not required to start treatment but helps exclude malignancy/infection.
📏 Diagnostic frameworks (support, don’t delay)
- 🧩 2016 EULAR/ACR sJIA–MAS criteria: ferritin ≥684 µg/L + ≥2 of ↓platelets, ↑AST, ↑triglycerides, ↓fibrinogen (within sJIA context).
- 🧮 HScore (adult sHLH) useful adjunct; do not wait to treat if high suspicion.
🏥 Immediate management (start now, refine later)
- 🆘 Resuscitation + sepsis cover: ABC, fluids, oxygen; early HDU/ICU if shock/organ failure. UK: follow local sepsis guideline and de-escalate with microbiology.
- 💊 Pulse steroids: methylprednisolone 30 mg/kg/day (max 1 g) IV for 1–3 days, then prednisolone 1–2 mg/kg/day with slow taper to response.
- 🧷 IL-1 blockade first-line in Still’s/sJIA-MAS: anakinra 2–10 mg/kg/day SC/IV (adults often 100 mg 6–24-hourly). Escalate dosing in severe disease.
- 🛡️ Ciclosporin A 2–6 mg/kg/day PO/IV if incomplete response or contraindications; monitor creatinine, BP, levels.
- 🧰 Refractory options (specialist MDT): IVIG 2 g/kg; JAK inhibitor (e.g., baricitinib); IFN-γ blockade (emapalumab) in selected sHLH; etoposide for malignancy-driven HLH under haematology.
- ⚖️ Anticoagulation is individualised (DIC vs thrombosis risk). Avoid NSAIDs in coagulopathy/hepatitis.
🧭 Monitoring & pitfalls (UK pearls)
- 📊 Daily trends: ferritin, platelets, fibrinogen, ALT/AST, triglycerides. Falling fibrinogen/platelets with rising ferritin = danger signal.
- 🧪 On tocilizumab, CRP may be low — trust ferritin/fibrinogen/platelets and clinical picture.
- 🩺 In SLE flares with new cytopenias + LFT/coag changes, actively screen for MAS.
- 🤝 Early MDT: rheumatology, haematology, ID/microbiology, ICU.
- 🧯 Keep antimicrobials until cultures and trajectory reassure; review daily with micro.
- 🦴 Steroid care: bone/GI protection, glucose checks; vaccinate when stable (avoid live vaccines on significant immunosuppression).
🏡 Discharge & follow-up
- 🧭 Slow steroid taper; maintain disease control (often ongoing anakinra or other biologic per underlying condition).
- 📝 Relapse plan & safety-net: return of fever, bleeding, confusion, new cytopenias.
- 🗓️ Labs weekly then space out: FBC, LFTs, fibrinogen, ferritin, CRP/ESR; BP/renal if on ciclosporin.
💡 Bottom line for juniors
In a Still’s/SLE patient who looks septic but doesn’t culture, with sky-high ferritin, falling ESR, and dropping platelets/fibrinogen — treat as MAS today: pulse steroids, add anakinra early, involve rheum/haem/ICU, and keep sensible sepsis cover until sure. Trends beat single numbers. ✅
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
