| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Herpes Simplex Encephalitis (HSV)
Related Subjects: |Herpes Varicella-Zoster (Shingles) Infection |Chickenpox Varicella Infection |Varicella Cerebral Vasculopathy |Herpes Viruses |Herpes Zoster Ophthalmicus (HZO) Shingles |MonkeyPox |Mumps |Measles |Rubella (German Measles) |Epstein-Barr Virus infection |Cytomegalovirus (CMV) infections |CMV retinitis infections |Toxoplasmosis
⚡ Key Clinical Pearl: Always treat suspected HSVE with IV Aciclovir if it’s in the differential. HSVE can mimic a middle cerebral artery (MCA) stroke but clues such as fever 🌡️, seizures ⚡, confusion 🌀, and temporal lobe changes on MRI 🧠 should raise suspicion. It occurs in about 1 per 3,000 stroke cases, meaning a typical UK stroke unit may see one case every 5–10 years.
🧠 About
- HSVE is the most serious form of herpes encephalitis, typically caused by HSV-1 in adults.
- Other viral causes include HSV-2 (more common in neonates) and rarely West Nile virus.
📊 Epidemiology
- Incidence: ~1 case per million per year.
- UK: ~50–100 cases annually, about half in patients >50 years old.
- Presentation can be fulminant with coma, or initially stroke-like ➝ deterioration over hours–days.
- Estimated 12–25 patients per year in the UK present as stroke mimics out of ~100,000 annual strokes.
🦠 Virology & Aetiology
- 90% of adults are seropositive for HSV-1 (latent in trigeminal ganglion).
- Reactivation may occur with stress, trauma, immunosuppression, sunlight ☀️, menstruation, or infection.
- Predilection for the temporal lobes and limbic system ➝ causes haemorrhagic necrosis 💉.
- Spread can be unilateral ➝ bilateral but asymmetric involvement.
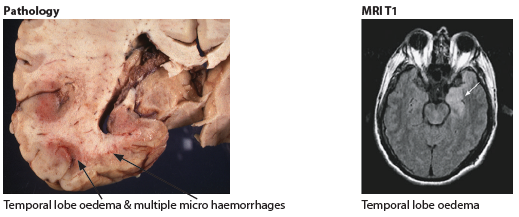
🧬 Pathology
- Haemorrhagic necrosis of the inferomedial temporal lobes.
- Limbic system involvement ➝ psychiatric changes, seizures, memory deficits.
- Histology: Cowdry Type A intranuclear inclusions in infected neurons.
🩺 Clinical Features
- Headache + fever + seizures ⚡
- Cold sores on lips or mouth (recent HSV reactivation) 👄
- Confusion, altered behaviour, personality change
- Speech abnormalities, focal deficits (hemiparesis, hyperreflexia)
- Severe cases: coma, raised ICP, death ☠️
- Can appear identical to a stroke with dysphasia and cognitive issues
🔍 Investigations
- FBC: Raised WCC.
- U&E: Hyponatraemia in ~50% (also seen in ~35% of strokes).
- CT/MRI: Temporal lobe oedema, necrosis, haemorrhage; restricted diffusion less intense than stroke.
- CSF: Lymphocytosis, ↑ protein, sometimes blood-stained. HSV PCR = gold standard.
- EEG: Focal temporal slowing, periodic discharges.
- Brain biopsy: Rare, but may show Cowdry A inclusions.
🖼️ Imaging Examples
📖 References
Cases — Herpes Simplex Encephalitis (HSV)
- Case 1 — Acute Confusion and Seizure: A 32-year-old woman presents with fever, headache, and a generalised tonic-clonic seizure. She is drowsy and disoriented. MRI brain: hyperintense lesions in the temporal lobe. CSF: lymphocytic pleocytosis, raised protein, normal glucose. Diagnosis: HSV encephalitis (classic temporal lobe involvement). Management: Immediate IV aciclovir; supportive neuro-ICU care; EEG monitoring if recurrent seizures.
- Case 2 — Psychiatric Presentation: A 24-year-old man develops acute personality change, bizarre behaviour, and hallucinations. No prior psychiatric history. He then develops fever and expressive dysphasia. Diagnosis: HSV encephalitis masquerading as acute psychosis. Management: Urgent IV aciclovir before confirmatory LP/PCR; neuro and psych liaison; seizure precautions.
- Case 3 — Elderly Patient with Delayed Diagnosis: A 70-year-old man is admitted with progressive confusion, fever, and focal seizures over 3 days. Initially treated as delirium. CT head normal, but MRI shows temporal lobe oedema with haemorrhagic change. CSF PCR: HSV-1 DNA positive. Diagnosis: HSV-1 encephalitis (delayed recognition). Management: High-dose IV aciclovir for 14–21 days; monitor renal function; rehabilitation for cognitive and speech deficits.
- Case 4 — Stroke Mimic in an Older Adult: A 68-year-old woman is brought to the ED with sudden-onset confusion, expressive aphasia, and right-sided weakness. Paramedics activated a stroke call. CT head shows no acute infarct. She spikes a fever in hospital and has a focal seizure. MRI reveals left temporal lobe oedema with haemorrhagic changes. CSF PCR is positive for HSV-1. Diagnosis: HSV encephalitis presenting as a stroke mimic (left temporal lobe involvement). Management: Immediate IV aciclovir; supportive care in neuro-ICU; speech and rehabilitation therapy post-acute phase.
Teaching Commentary 🧠
HSV encephalitis is the most common cause of sporadic fatal viral encephalitis, classically due to HSV-1 (HSV-2 more in neonates). Hallmarks: - Fever, headache, confusion, seizures. - Predilection for temporal lobes → dysphasia, hallucinations, behavioural changes. - MRI: temporal lobe hyperintensity ± haemorrhage. - CSF: lymphocytes, ↑protein, normal glucose; PCR confirms HSV. Immediate IV aciclovir should be started empirically (delay worsens prognosis). Complications: seizures, long-term cognitive impairment. Mortality untreated ≈70%, but with treatment ≈20%.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
