| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Burns Management Guide
Related Subjects: |Cellulitis |Pyoderma gangrenosum |Pemphigus Vulgaris |Toxic Epidermal Necrolysis |Stevens-Johnson Syndrome |Necrotising fasciitis |Gas Gangrene (Clostridium perfringens) |Purpura Fulminans |Severe burns |Anatomy of Skin
| 🛠️ Initial Management of Severe Burns: Always Look for Secondary Injuries |
|---|
|
🔥 Anyone with burns should also be presumed to have smoke inhalation injury — consider the ABCs and watch for stridor, hoarseness, or drooling. 😮💨 These patients are at risk for ARDS and airway compromise, which may require early intubation. 📞 Referral: Transfer to a burns centre if:
- 👶 >10% TBSA in children
- 🧑 >15% TBSA in adults
- 🩹 Any full-thickness burns
- 😷 Burns to face, hands, perineum, feet, flexures, or joints
- ⚡ Chemical, electrical, lightning injuries
- 🔥 Circumferential limb or chest burns
- 🚨 Suspected inhalation injury
🔥 Types of Burns
- ☀️ First Degree / Superficial: Epidermis only. Red, painful, no blisters. Heal without scarring.
- 💧 Second Degree / Partial Thickness: Epidermis + dermis. Red, blistered, very painful, moist. Heal with minimal scarring.
- 🪵 Third Degree / Full Thickness: All layers destroyed. White/charred/leathery. Painless (nerve damage). Needs grafting → scarring.
😷 Signs of Inhalational Injury
- Facial/neck/chest burns
- Singed nasal hair/eyebrows
- Soot in sputum/oropharynx
- Hoarseness, stridor, dyspnoea
- Oropharyngeal swelling/erythema
⚠️ Complications of Burns
- Compartment syndrome
- Hypovolaemia, electrolyte imbalance
- Infection, sepsis
- Hypothermia
- Neuropathic pain, pruritus
- Hypertrophic scars, contractures
- Psychological trauma: depression, anxiety, PTSD
📍 Special Areas of Concern
- Face, hands, perineum, genitalia, feet, flexures, joints → functional & cosmetic impact.
🧪 Investigations
- Bloods: FBC, U&E, glucose, clotting, CK, cross-match
- ABG: lactate, HbCO
- CXR if inhalation suspected
🧾 Management Overview
- ABCDE approach 🔄
- High-flow O₂ 💨
- Fluid resuscitation 💧 (Parkland + urine monitoring)
- Early intubation if airway risk 🫁
- Wound care: cling film, sterile dressings 🩹
- IV analgesia 💊
- Nutritional support 🍲 (↑ metabolic demand, dietician input)
- Escharotomy if needed ✂️
- Tetanus prophylaxis 💉
- Early burns unit referral 📞
📚 Teaching Commentary
Burns are a multisystem insult — airway, circulation, and metabolism all collapse if not managed promptly. The first 24h = airway + fluids, not definitive surgery. Always check for “hidden killers”: inhalational injury, CO or cyanide, associated trauma. UK practice: 🔗 burns care is regionalised → early referral is life-saving. Remember: 🧪 resuscitation is a balance — underdo it and they die of shock, overdo it and you worsen oedema, including airway swelling. And never forget the patient’s psychological and safeguarding needs — scarring and trauma can last far beyond the acute injury.
🔖 References
- ABC of Burns: Pathophysiology and Types of Burns
- Clinical Guideline: Burns Injury
- Management of Major Burns: A Review
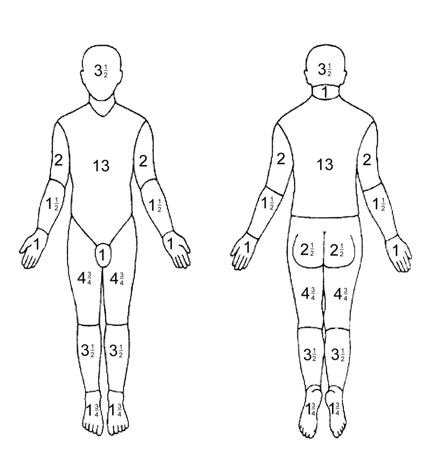
Case 1 – Adult flame burn with inhalation risk
A 38-year-old rescued from a house fire has facial burns, singed nasal hairs, hoarse voice, and cough with soot; mixed-depth burns to the anterior trunk and both upper limbs (~28% TBSA, Rule of Nines). Priorities: ABCDE with high-flow O₂ (100% non-rebreathe), early airway protection if progressive oedema/stridor, and blood gases including carboxyhaemoglobin (pulse oximetry unreliable). Start warmed IV fluids using the Parkland formula (4 mL/kg/%TBSA of lactated Ringer’s; give half in 8 h from time of burn), titrating to urine ≥0.5 mL/kg/h; insert urinary catheter and consider analgesia, tetanus, and escharotomy if circumferential chest/limb burns impair ventilation/flow. Cool the burn (20 min tepid water if <3 h from injury), cover with cling film, avoid ice. Refer to a UK burns centre (e.g., >10% TBSA, face/airway, hands/perineum, electrical/chemical, or inhalation injury) for debridement and definitive dressings/grafting.
Case 2 – Paediatric scald; safeguarding considerations
A 2-year-old pulls a kettle lead causing hot-water scald to the anterior chest and left arm; blistered, painful partial-thickness burns covering ~8% TBSA (use Lund–Browder chart). Manage with ABCDE, prompt analgesia (oral morphine/IN fentanyl as appropriate), tepid cooling for up to 20 min, non-adherent dressing (paraffin gauze) and cling film, elevation of the limb, and oral fluids ± IV if not tolerating; consider fluid resuscitation if >10% TBSA (many UK centres use 2–3 mL/kg/%TBSA in children) and maintain euglycaemia. Assess tetanus status. Document a careful history and injury pattern; involve senior review and safeguarding if concerns (e.g., clear immersion lines, inconsistent story). Arrange burns clinic follow-up within 24–48 h to monitor pain, infection, and function; early physiotherapy/splinting if joints are involved.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
