| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Aortic Dissection
Related Subjects: |Assessing Chest Pain |Acute Coronary Syndrome (ACS) General |Aortic Dissection |Pulmonary Embolism |Acute Pericarditis |Diffuse Oesophageal Spasm |Gastro-oesophageal reflux |Oesophageal Perforation Rupture |Pericardial Effusion Tamponade |Pneumothorax |Tension Pneumothorax |Shingles | Ankle-Brachial pressure Index (ABPI) and Peripheral Vascular Disease | Peripheral Arterial Disease (PAD) | Abdominal Aortic Aneurysm (AAA) | Carotid Endarterectomy | Buerger's disease (Thromboangiitis obliterans ) | Leriche syndrome (aortoiliac occlusive disease)
🚨 The most critical step is to consider aortic dissection in any patient with chest pain — misdiagnosis as MI ❤️🔥 or PE 🩸 is dangerous, since anticoagulation increases the risk of fatal bleeding. Early recognition + urgent referral are lifesaving.
| 🩺 Management of Acute Aortic Dissection |
|---|
|
🤰 Consider dissection in pregnancy and postpartum chest pain (with PE). 🖥️ POCUS can be lifesaving at bedside.
📖 About Aortic Dissection
- Mortality: ~40% die at onset ⚰️; another 10% peri/post-op.
- Urgent CT Aortogram essential 🖥️.
- Type A = surgery; Type B = medical management.
- Beta-blockade crucial to reduce shear stress 💊.
- Chronic dissection (rare) → ongoing pain, HF signs.
🧬 Aetiology
👶 Young patients: connective tissue disorders (e.g. Marfan, Ehlers–Danlos). 👴 Older patients: hypertension, atherosclerosis.
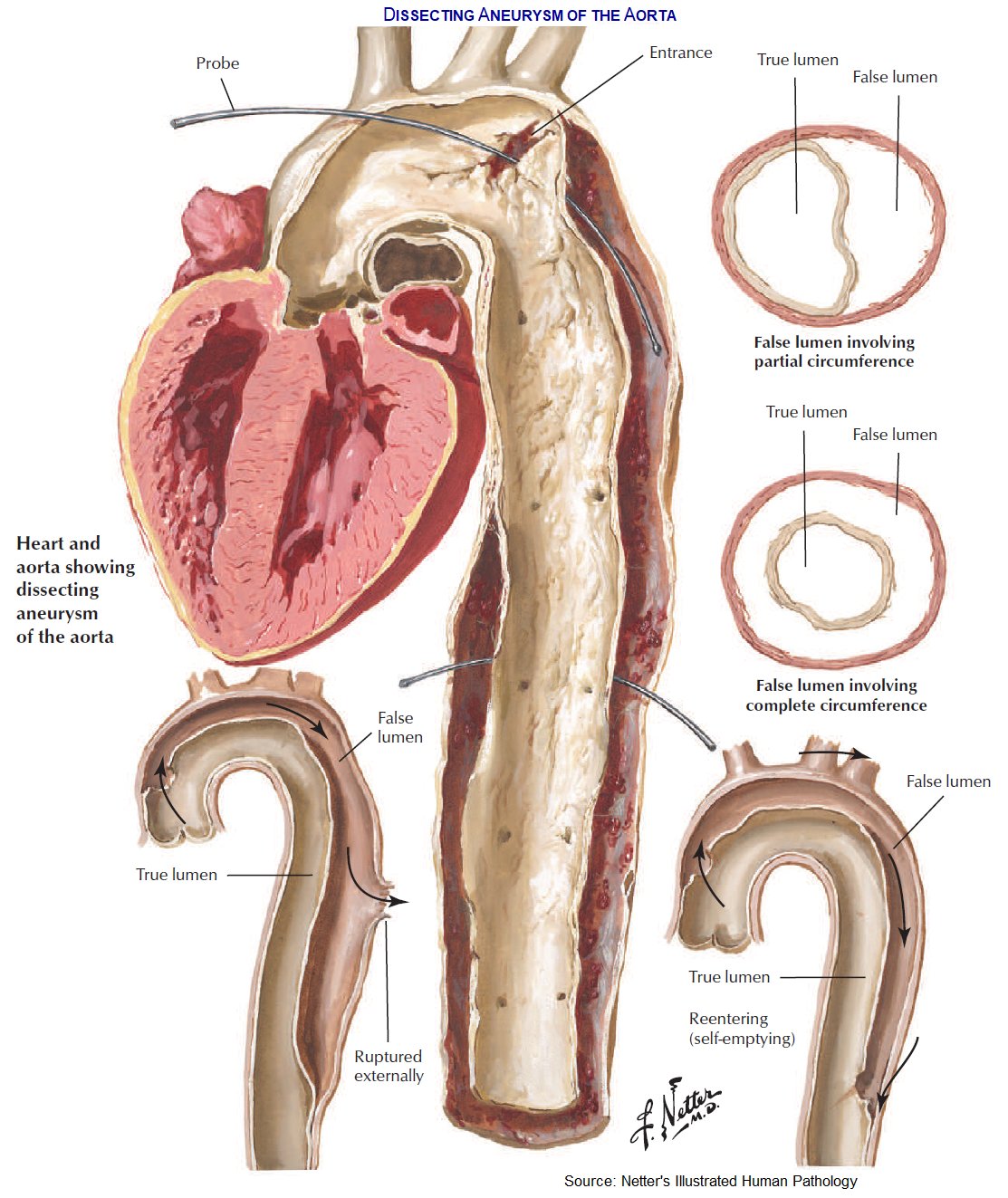
- Aortic wall layers: intima, media, adventitia.
- Tear in intima → blood into media → false lumen forms.
- Extensions: ➡️ Antegrade → distal vessels 🫀 ⬅️ Retrograde → valve, coronaries, tamponade 💧 💥 Rupture → haemothorax, sudden death 🔁 Re-entry → stabilisation possible
 <
<
🗂️ Classification
- Stanford: • Type A = ascending aorta (2/3 cases) ⚡ → surgery • Type B = descending aorta → medical
- DeBakey: • I = Ascending + arch/descending • II = Ascending only • III = Descending only
⚠️ Risk Factors
- ♂ > ♀, >60 yrs
- Hypertension, atherosclerosis
- Connective tissue disorders 🧬
- Trauma, bicuspid AV, prior surgery
- Cocaine use 💊, pregnancy 🤰
- Aortitis (Takayasu, GCA) 🧪
🩺 Clinical Presentation
- Sudden tearing chest pain radiating to back ⚡🖤
- Shock or hypertension, different BP between arms 💪
- Aortic regurg murmur + pulmonary oedema 🌊
- Syncope (~15%) due to tamponade/major vessel occlusion
❗ Complications
- Type A: Tamponade 💧, rupture 💥, AR → HF, stroke 🧠
- Type B: Spinal stroke 🦽, mesenteric/renal ischaemia ⚠️, haemothorax 🫁
🔎 Investigations
- Bloods: U&E, FBC, group & crossmatch 💉
- CXR: widened mediastinum 📏, left pleural effusion
- ECG: may mimic MI (if RCA involved) ❤️🔥
- D-dimer: often ↑, normal helps exclude ❌
- CT Aortogram = gold standard 🖥️
- TOE: rapid diagnosis if unstable
🛠️ Management
- ABC + monitoring ⚡
- Pain: IV morphine 💊
- Lower BP: IV labetalol (± nitroprusside) ⬇️
- Type A = 🚑 surgery (mortality rises 1–2% per hr delay!)
- Type B = strict BP control + endovascular stent (TEVAR) where indicated
📚 References
🧑⚕️ Case Examples — Aortic Dissection
- Case 1 (Type A — ascending aorta): 💔 A 58-year-old man with poorly controlled hypertension presents with sudden severe “tearing” chest pain radiating to the back. He is diaphoretic, with unequal arm BPs. ECG is non-diagnostic, troponin normal. Analysis: Classic Type A dissection involving the ascending aorta — high mortality if untreated. Diagnosis: CT angiography confirms Stanford Type A dissection. Management: Immediate BP control with IV labetalol, urgent cardiothoracic surgical repair.
- Case 2 (Type B — descending aorta): 🫀 A 70-year-old woman with long-standing hypertension and COPD develops sudden tearing interscapular back pain. BP is 210/110, both arms equal. No signs of end-organ malperfusion. Analysis: Stanford Type B dissection (distal to left subclavian artery). Often managed medically if uncomplicated. Diagnosis: CT angiogram shows descending thoracic aortic dissection. Management: Aggressive BP control (IV beta-blocker, vasodilator), pain relief, monitoring. Surgery/endovascular stent reserved for complications (rupture, malperfusion, uncontrolled pain/HTN).
- Case 3 (Complicated dissection with malperfusion): 🚨 A 65-year-old man with Marfan’s syndrome presents with severe chest pain, syncope, and left leg weakness. On exam: BP 90/60, reduced left femoral pulse, new diastolic murmur. Analysis: Aortic dissection complicated by branch vessel involvement (left iliac, aortic regurgitation, possible tamponade). Diagnosis: Stanford Type A dissection with end-organ compromise. Management: Resuscitation, IV beta-blockade, urgent surgical repair. Prognosis poor without immediate intervention.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
