| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Head Injury and Traumatic Brain Head Injury (TBI)
Related Subjects: |Initial Trauma Assessment and Management |Thoracic Trauma Assessment and Management |Head Injury and Traumatic Brain Head Injury (TBI) |Flail Chest Rib fractures |Resuscitative Thoracotomy |Haemorrhage control |Traumatic Head/Brain Injury |Traumatic Cardiac Arrest |Abdominal trauma |Tranexamic Acid |Silver Trauma |Cauda Equina |Adult Resus:Basic Life Support |Adult Resus: Advanced Life Support |Resus:Acute Haemorrhage
🧠 Head injury is the most common cause of death and disability in people aged 1–40 in the UK. Refer to NICE guidance (all ages). Red flag triggers for CT: GCS < 15, LOC, focal neurology, suspected skull fracture, amnesia, persistent headache, vomiting, seizures, anticoagulant use (except aspirin alone), high-energy mechanism, or safeguarding concerns.
ℹ️ About
- 💥 Trauma to scalp, skull, or brain (excludes superficial face injuries).
- 🚗 Common causes: RTAs, falls, assaults (age & geography dependent).
- 🔒 Classified as closed (no fracture) or penetrating (with fracture).
- 📊 Accounts for ~7% of major trauma; ~5% mortality.
- ⚡ Early neuroprotective care significantly improves outcome.
Epidemiology
- 🏥 10% of A&E attendances; 25% admitted.
- Only 1% referred to neurosurgery.
- 👨 Young men highest risk; bimodal peaks in young adults and elderly.
- Head injuries = 50% of trauma deaths; 60% from RTAs.
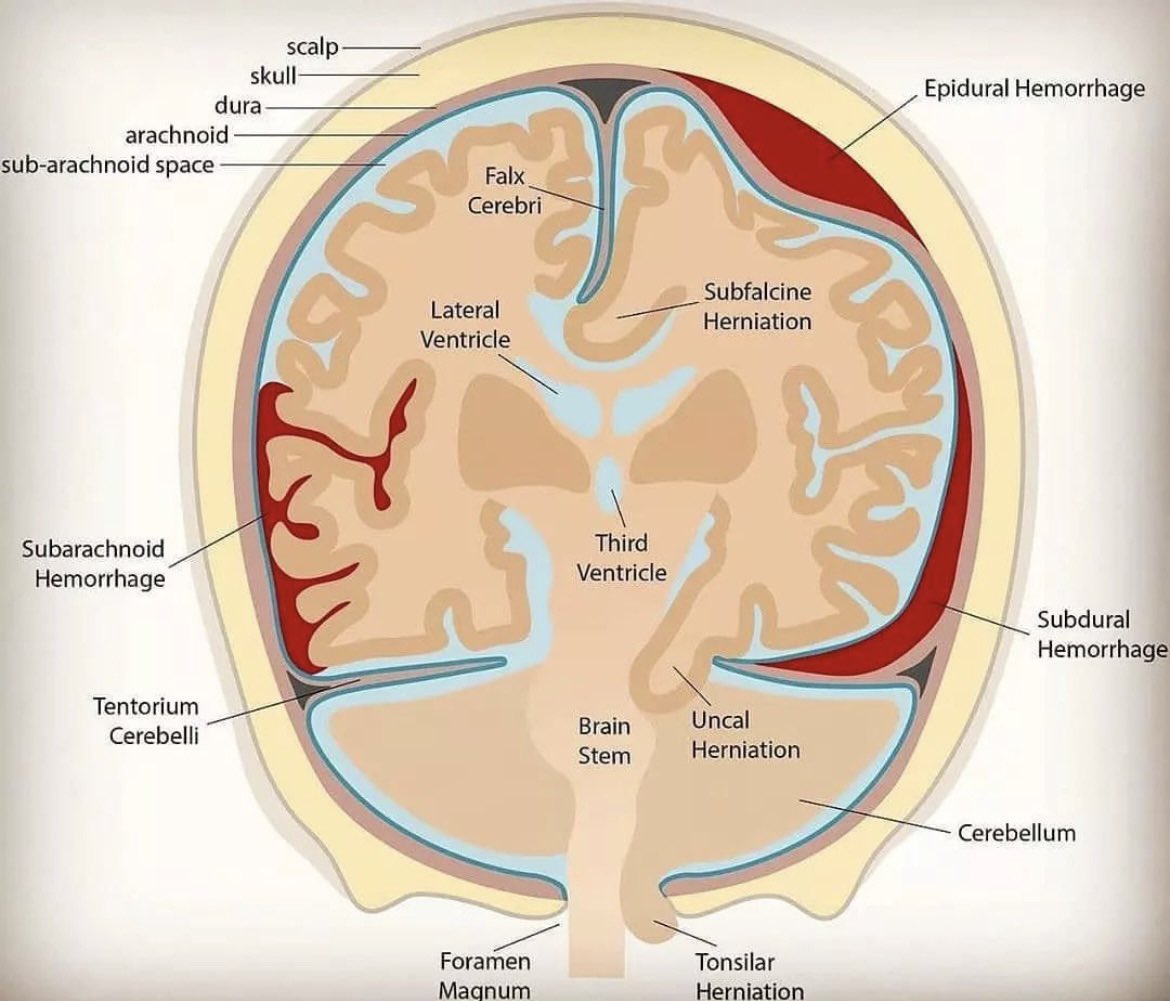
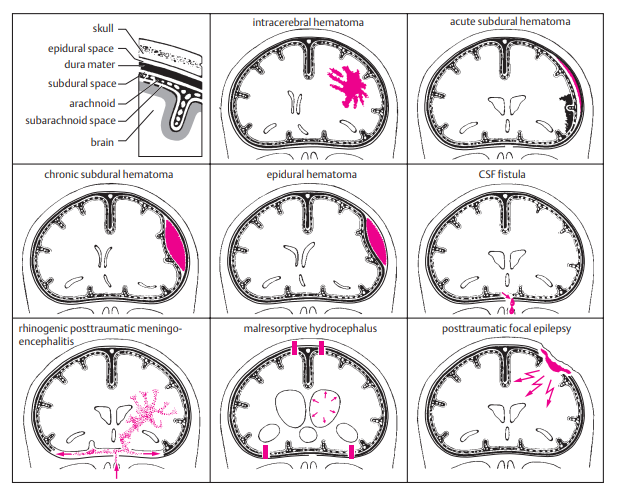
Patterns of Brain Bleeds
Mechanism of Injury
- ⚡ Direct trauma → axonal shearing, contusions, haemorrhage.
- 🧩 Primary injury: occurs at time of impact (contusions, DAI, lacerations).
- ♻️ Secondary injury: hypoxia, raised ICP, oedema, haematoma, seizures, infection.
- High-risk events: high-speed RTA, fall ≥3m, elderly fall, alcohol, altered GCS.
Risk Factors & Concerns
- 🧑🤝🧑 Groups: young men (15–29), elderly, RTAs, falls, assaults.
- By bleed type:
- 🩸 Subdural haematoma → elderly, bridging vein rupture.
- 🩸 Extradural haematoma → young, MMA rupture, lucid interval.
- 🩸 Traumatic ICH / SAH → diffuse, often with contusions.
Clinical Assessment (ABCDE + Neuro)
- 📍 Mechanism, LOC, amnesia, seizure, vomiting.
- 🧍 Full GCS & neuro exam (limbs, pupils, vision, speech).
- 👁️ Pupil dilatation + coma = brainstem compression until proven otherwise.
- 💧 CSF leak from nose/ear = base of skull fracture (check for “panda eyes” or Battle’s sign).
- 🔎 Always assess for associated trauma (C-spine, chest, long bones).
Investigations (NICE CT Criteria)
- 🕐 CT Head within 1h if:
- GCS < 13 initially or < 15 at 2h
- Open/depressed skull fracture
- Signs of base of skull fracture
- Seizure, focal deficit
- ≥1 vomiting episode
- 🕗 CT Head within 8h if:
- Age ≥ 65
- Bleeding/clotting disorder or anticoagulant/antiplatelet (except aspirin alone)
- Dangerous mechanism (ejected, fall ≥1m)
- Retrograde amnesia > 30 mins
Complications of Head Injury
| Complication | Mechanism | Clues | Management |
|---|---|---|---|
| Intracranial Haemorrhage | Arterial/venous rupture | Deteriorating GCS, focal signs | Urgent CT, craniotomy, ICP control |
| Diffuse Axonal Injury | Shearing | Low GCS, normal CT | ICU, ICP monitor, rehab |
| Skull Fractures | Linear, depressed, basilar | CSF leak, Battle’s sign, cranial nerve palsy | CT, repair if needed, meningitis prophylaxis |
| Seizures | Cortical irritability | Early or late seizures | Levetiracetam 1g BD; prophylaxis in severe |
| Cerebral Oedema | Raised ICP | Bradycardia, hypertension, irregular RR (Cushing’s) | Mannitol, hypertonic saline, hyperventilation, decompression |
| Hydrocephalus | CSF obstruction | Headache, vomiting, papilloedema | Ventriculostomy/shunt |
| PCS | Concussion | Persistent headache, poor concentration | Symptom control, neuro rehab |
| CTE | Repetitive trauma | Memory decline, behavioural change | Supportive, long-term rehab |
Infographic
💊 Management
- 🩺 ABCDE first: oxygen (SpO₂ 94–98%), 2x IV access, C-spine precautions.
- 💤 GCS ≤ 8 → intubate (call anaesthetist, RSI with neuroprotective sequence).
- 🧾 Urgent CT head/neck if indicated.
- 💉 Reverse anticoagulation (target platelets ≥100).
- 👀 Obs: GCS, pupils, vitals — half-hourly ×2h → hourly ×4h → 2-hourly if stable.
- 📌 Neurosurgical referral if: GCS ≤8, deteriorating GCS, new focal signs, abnormal CT.
- 💊 Seizure prophylaxis: Levetiracetam 1g BD IV → NG/PO when possible.
- 🤝 Long-term: early neuro-rehabilitation (OT, physio, psychology).
🌟 Exam tip: - Extradural = lucid interval, young patient, MMA tear. - Subdural = elderly, bridging veins, gradual decline. - DAI = normal CT but low GCS.
References
🧾 Clinical Case Examples
Case 1 – Extradural haematoma ⚡
A 21-year-old motorcyclist, not wearing a helmet, falls off his bike. He loses consciousness briefly, then is lucid for 1 hour before suddenly collapsing. On exam: right fixed dilated pupil, left-sided weakness.
👉 Diagnosis: Extradural haematoma (middle meningeal artery rupture).
👉 Management: Urgent CT head, neurosurgical referral for craniotomy.
Case 2 – Subdural haematoma 🩸
An 80-year-old woman on warfarin trips at home and strikes her head. Over the next 2 days she becomes confused and drowsy. GCS drops from 15 → 12.
👉 Diagnosis: Acute-on-chronic subdural haematoma (bridging vein rupture).
👉 Management: CT head, reverse anticoagulation, neurosurgical discussion.
Case 3 – Diffuse axonal injury 🧩
A 19-year-old student is involved in a high-speed RTA. At the scene his GCS is 6. In ED: intubated, CT head appears normal.
👉 Diagnosis: Diffuse axonal injury.
👉 Management: Admit to ICU, ICP monitoring, supportive neurocritical care, later rehabilitation.
Case 4 – Base of skull fracture 💧
A 35-year-old man is assaulted. He presents with periorbital bruising (“raccoon eyes”) and clear fluid leaking from the ear.
👉 Diagnosis: Basilar skull fracture with CSF leak.
👉 Management: CT head + temporal bones, neurosurgical review, prophylactic antibiotics not routinely given (unless advised by specialist), monitor for meningitis.
Case 5 – Post-concussion syndrome 🌀
A 28-year-old woman presents 2 weeks after a minor head injury. She complains of persistent headaches, poor concentration, irritability, and disturbed sleep. GCS was 15 at the time of injury, CT normal.
👉 Diagnosis: Post-concussion syndrome.
👉 Management: Reassurance, symptom control (analgesia, sleep hygiene), occupational health/psychology support if prolonged.
Case 6 – Anticoagulated head injury 💊
A 72-year-old man on apixaban falls in the bathroom, striking his head. He is GCS 15 with no focal neurology.
👉 Diagnosis: High-risk head injury on anticoagulation.
👉 Management: CT head within 1h (NICE), consider reversal if bleed, admit for observation even if initial CT normal.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
