| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Motor Neuron Disease (MND-ALS)
Related Subjects: |Neurological History taking |Motor Neuron Disease (MND-ALS) |Miller-Fisher syndrome |Guillain Barre Syndrome |Multifocal Motor Neuropathy with Conduction block |Multiple Sclerosis (MS) Demyelination |Inclusion Body Myositis |Cervical spondylosis |Anterior Spinal Cord syndrome |Central Spinal Cord syndrome |Brown-Sequard Spinal Cord syndrome |Spinal Cord Compression |Spinal Cord Haematoma |Spinal Cord Infarction
🧠 Motor Neurone Disease (MND) presents with generalized and bulbar weakness, muscle wasting, brisk reflexes, and no sensory loss. Eye and bladder function are typically spared. ⚡ There is no definitive diagnostic test — diagnosis relies on clinical signs involving both the brain and spinal cord.
ℹ️ About
- Also known as Amyotrophic Lateral Sclerosis (ALS), Charcot's disease, and Lou Gehrig's disease.
- ⏳ Diagnosis is often delayed, sometimes taking >16 months from symptom onset.
- Initial symptoms may be vague, e.g., fatigue or weakness.
How Common Is It? 📊
- Incidence: 1.8–2.2 per 100,000 population.
- Prevalence: 4.0–4.7 per 100,000 population in the UK.
- At any given time, ~2,000 individuals in England and Wales are affected.
Pathology 🔬
- Degeneration of motor giant pyramidal Betz cells (layer V, primary motor cortex).
- Loss of anterior horn cells in the spinal cord.
- Degeneration of cranial motor nuclei in the brainstem.
Aetiology / Genetics 🧬
- 🌍 Guam variant: linked with dementia & parkinsonism in the Chamorro people.
- SOD1 mutations implicated in familial ALS.
- Other mutations: RNA processing, axonal transport, cytoskeletal proteins.
- Familial ALS = ~10% of cases, usually autosomal dominant.
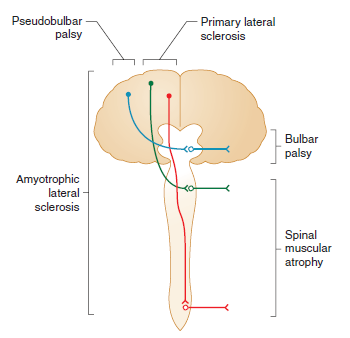
Forms of MND 🧾
- Progressive Muscular Atrophy: LMN predominant. ⏳ Survival 5–10 yrs.
- Progressive Bulbar Palsy: Tongue wasting, fasciculations, spastic palate. ⏳ Survival 2–3 yrs.
- Primary Lateral Sclerosis: UMN predominant, symmetrical. 👍 Good prognosis.
- ALS: UMN + LMN features. ⏳ Survival 3–4 yrs.
- MND-Dementia: Associated with FTD (frontotemporal dementia).
Clinical Features ⚠️
- 💪 Subtle weakness → progresses to wasting & fasciculations (esp. hands).
- 🌙 Painful nocturnal cramps (thighs common).
- Mixed UMN + LMN signs: weakness + brisk reflexes + extensor plantar.
- 🙅♂️ No significant sensory loss; eye movements & sphincters spared.
- 👅 Bulbar involvement: wasted fibrillating tongue, dysarthria, dysphagia.
- ⚖️ Weight loss due to dysphagia & wasting.
- “Dropped head” & wasted hands appearance.
El Escorial Criteria 📋
- Clinically Definite ALS: UMN + LMN signs in ≥3 regions (bulbar, cervical, thoracic, lumbar).
- Clinically Probable ALS: UMN + LMN in 2 regions, UMN above LMN.
- Clinically Possible ALS: UMN + LMN in 1 region only.
Differential Diagnosis 🔍
- MMN with conduction block (check GM-1 antibodies).
- Cervical spondylotic myelopathy, foramen magnum lesions (MRI).
- CIDP, Inclusion Body Myositis.
- Myasthenia Gravis (Tensilon, antibodies, EMG).
- Kennedy’s syndrome (X-linked).
- B12 deficiency, Lyme disease, malignancy.
Investigations 🧪
- FBC, U&E, TFT, CK, syphilis serology.
- CSF: may show mild ↑ protein.
- Autoantibody panel (exclude mimics).
- MRI brain/cervical spine → rule out mimics (syrinx, compression, vascular).
- EMG: fasciculations + fibrillation (LMN loss).
- Nerve conduction: often normal until late.
Management 🩺
- 👩⚕️ Multidisciplinary Support: Physio, OT, SALT, dietician, palliative input.
- 💊 Riluzole 50mg bd: Glutamate antagonist → extends survival by ~2–3 months.
- 💧 Anticholinergics: Glycopyrrolate, amitriptyline, or hyoscine for drooling.
- 🦵 Baclofen / Diazepam: Spasticity control.
- 🥤 Feeding support: NG, PEG, or RIG feeding when bulbar involvement advances.
- 😴 NIV (BiPAP): Improves sleep, reduces fatigue, ↑ survival by ~6 months.
- 🗣️ Speech synthesizers: Assist communication.
- 💊 Quinine, Carbamazepine, Gabapentin → muscle cramps.
- 🙂 SSRIs or mood stabilisers for depression & emotional lability.
Prognosis 📉
- Median survival: 2–3 yrs from diagnosis.
- ~25% survive ≥5 yrs.
References 📚
Cases — Motor Neurone Disease (MND)
- Case 1 — Amyotrophic Lateral Sclerosis (ALS, Mixed UMN & LMN) ⚡: A 58-year-old man presents with progressive weakness in his right hand, muscle fasciculations, and stiffness in his legs. Exam: wasting of hand intrinsic muscles, brisk reflexes, extensor plantar responses. No sensory loss. Diagnosis: ALS (most common form of MND). Management: Riluzole to modestly extend survival; physiotherapy; MDT input; NIV (non-invasive ventilation) for respiratory support.
- Case 2 — Progressive Bulbar Palsy 🗣️: A 62-year-old woman presents with slurred speech, difficulty swallowing, and choking on liquids. Exam: tongue wasting with fasciculations, brisk jaw jerk, nasal dysarthria. Diagnosis: Bulbar-onset MND (progressive bulbar palsy). Management: MDT care; speech and language therapy; gastrostomy for nutrition; NIV; symptomatic treatment of sialorrhoea.
- Case 3 — Primary Lateral Sclerosis (PLS, UMN-Predominant) 🧠: A 50-year-old man presents with progressive leg stiffness and spastic gait over 3 years. Exam: pyramidal weakness, brisk reflexes, extensor plantar responses, but no fasciculations or wasting. Sensation intact. Diagnosis: Primary lateral sclerosis (UMN-predominant MND variant). Management: Supportive — physiotherapy, spasticity control (baclofen, tizanidine), MDT monitoring.
Teaching Commentary 🧠
MND is a group of progressive neurodegenerative disorders of upper and lower motor neurones. - ALS: UMN + LMN signs, most common. - Bulbar Palsy: speech and swallowing first; poorer prognosis. - PLS: UMN-predominant; slower progression. - PMA (progressive muscular atrophy): LMN-predominant. Clues: weakness with fasciculations, mixed UMN/LMN signs, no sensory loss, progressive. Dx: clinical + EMG (denervation); MRI excludes mimics. Mx: Riluzole, multidisciplinary care, NIV, gastrostomy, palliative support. Prognosis: average survival 2–5 years (longer in PLS).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
