| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Air Embolism
Related Subjects: | Air Embolism
💨 Air Embolism occurs when air bubbles enter the bloodstream, obstructing circulation. This can happen during surgery, trauma, medical procedures, or diving accidents 🏊♂️. The severity depends on the volume of air and site of obstruction, with potential for life-threatening complications. 📌 Positioning the patient: Place head down + left side down (left lateral decubitus, Trendelenburg) → traps air in the right ventricular apex, slowing systemic entry.
📌 About Air Embolism
- ⚙️ Mechanism: Air enters venous or arterial circulation → obstructs blood flow → impaired perfusion.
- 🫀 Venous Air Embolism (VAE): Air reaches right heart → pulmonary artery blockage → hypoxia & cardiovascular collapse.
- 🤿 Divers & Decompression: Rapid ascent → nitrogen bubbles (decompression sickness) mimics air embolism.
- ⚠️ Severity: Even 0.5–1 mL in coronary/cerebral arteries can be fatal; 50 mL+ venous air can cause cardiovascular collapse.
🔬 Pathophysiology
- 🩸 Venous entry favoured when site above right atrium → negative venous pressure sucks in air.
- 🚪 Arterial embolism may arise from pulmonary barotrauma or paradoxical embolism via PFO/ASD.
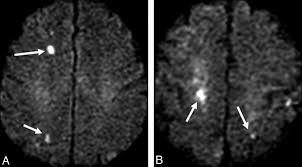
- 🧠 Cerebral and coronary circulation are most vulnerable → stroke-like deficits or MI.
📋 Causes
- 🩻 Surgical Procedures: Neurosurgery, cardiothoracic surgery, or central line manipulation.
- 🪓 Trauma: Chest/neck penetrating injuries or fractured veins.
- 💉 Central Lines & Catheters: Insertion/removal mishaps → most common iatrogenic cause.
- 🤿 Diving Accidents: Poor decompression control → nitrogen embolism/air embolism overlap.
- 💨 Positive Pressure Ventilation: Barotrauma → alveolar-vascular air entry.
🧾 Types
- 🫀 Venous Air Embolism (VAE): → Right heart & lungs → pulmonary hypertension, hypoxia, RV strain.
- 🧠 Arterial Air Embolism (AAE): → Brain, heart, kidneys → stroke, MI, multiorgan injury.
⚠️ Clinical Signs
- 😮 Dyspnoea, hypoxia, cyanosis
- ❤️ Chest pain, arrhythmias
- 🧠 Neurological deficits → dizziness, seizures, confusion, focal stroke
- 📉 Hypotension, obstructive shock
- 💔 Cardiac arrest in severe cases
🔎 Investigations
- 🧪 ABG: Hypoxia ± metabolic acidosis.
- 📈 ECG: RV strain, tachycardia, ST changes.
- 🩻 CXR: Non-specific; may show pulmonary oligemia.
- 🫀 TEE: Sensitive → visualises air bubbles in right atrium/ventricle.
🩺 Differentials
- PE 🫁
- Stroke / TIA 🧠
- MI ❤️
- Tension pneumothorax 🫁
- Cardiac tamponade 💔
🚨 Complications
- 💔 Cardiac arrest (obstructive shock)
- ❤️ Myocardial infarction (coronary embolism)
- 🧠 Hypoxic brain injury (cerebral embolism)
- 🫁 ARDS & respiratory failure
🛡️ Prevention
- 🏥 Procedures: Careful central line insertion/removal, IV filters.
- 🤿 Divers: Controlled ascent & decompression stops.
- 💉 Hospital: Positioning during catheter removal, air-tight line handling.
⚕️ Management
- 🔄 Resuscitation: ABCs, 100% high-flow O₂ (non-rebreather).
- 🛏️ Position: Left lateral decubitus + Trendelenburg.
- 🤐 Intubation/Ventilation: For severe hypoxia.
- 💧 Fluids ± Inotropes: To maintain preload and cardiac output.
💡 Advanced Management
- 💉 Aspiration: Via central venous catheter in RA if accessible.
- 🌊 Hyperbaric Oxygen Therapy (HBOT): Shrinks bubbles, improves oxygenation; gold standard in cerebral/cardiac involvement.
- 🔪 Open Chest Aspiration: Rare; in intra-op cases, direct removal of air from RV or pulmonary artery.
📉 Prognosis
- ⏱️ Depends on speed of recognition & management.
- ✅ Early O₂ + positioning can reverse symptoms.
- ❌ Delayed treatment → permanent neurological injury or death.
📚 References
Case – Venous air embolism after central line removal
A 62-year-old on a surgical ward becomes acutely dyspnoeic and hypotensive minutes after removal of a right IJ central line; she is upright when the dressing lifts and a hissing sound is heard. On exam: tachycardia, hypoxia, raised JVP, and a fleeting “mill–wheel” precordial sound; bedside echo shows RV strain without thrombus. Suspect venous air embolism precipitated by negative intrathoracic pressure. Immediate actions: 100% oxygen (reduces bubble size & treats shunt), place in left lateral decubitus with slight Trendelenburg (Durant’s), apply occlusive pressure dressing over the insertion site, support circulation (IV fluids/vasopressors) and call ICU; if a central line remains, attempt aspiration of air from the right heart. Consider hyperbaric oxygen urgently if neurological deficits or coronary/cerebral involvement suggest arterial gas embolism. Differentiate from PE and tension pneumothorax. Prevention: remove lines with the patient supine/Trendelenburg, during end-expiration or Valsalva, maintain firm occlusive pressure for ≥5–10 min, and use an airtight dressing.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
