| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Alzheimer disease (Dementia)
Related Subjects: |Behavioural and Psychological (BPSD) Symptoms of Dementia |Alzheimer disease (Dementia)
🧠 Alzheimer’s Disease (AD) = the commonest cause of dementia, affecting ~10% of people >65. Characterised by progressive cognitive decline, memory loss, and behavioural changes. Diagnosis is clinical, supported by cognitive testing, imaging, and history.
ℹ️ About
- Diagnosis = patient/family history + cognitive testing + exam + imaging.
- ⚠️ Progressive decline in cognition & daily function.
- Common in older age; prevalence increases markedly >80 yrs.
🧬 Aetiology
- Increased prevalence in Down syndrome (chromosome 21 link).
- Genetic link to apolipoprotein E4.
- Pathophysiology: reduced cholinergic, noradrenergic, dopaminergic activity.
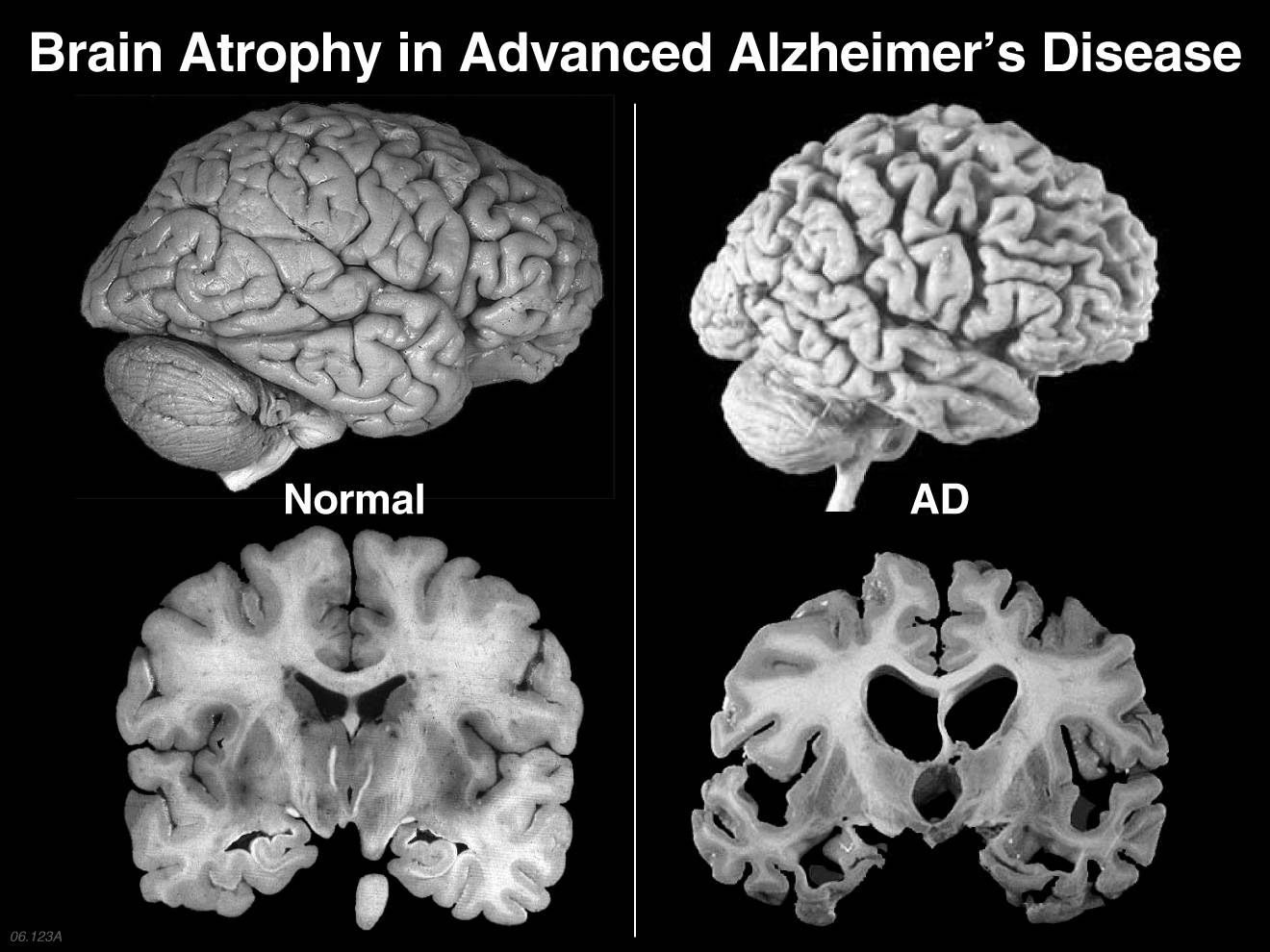
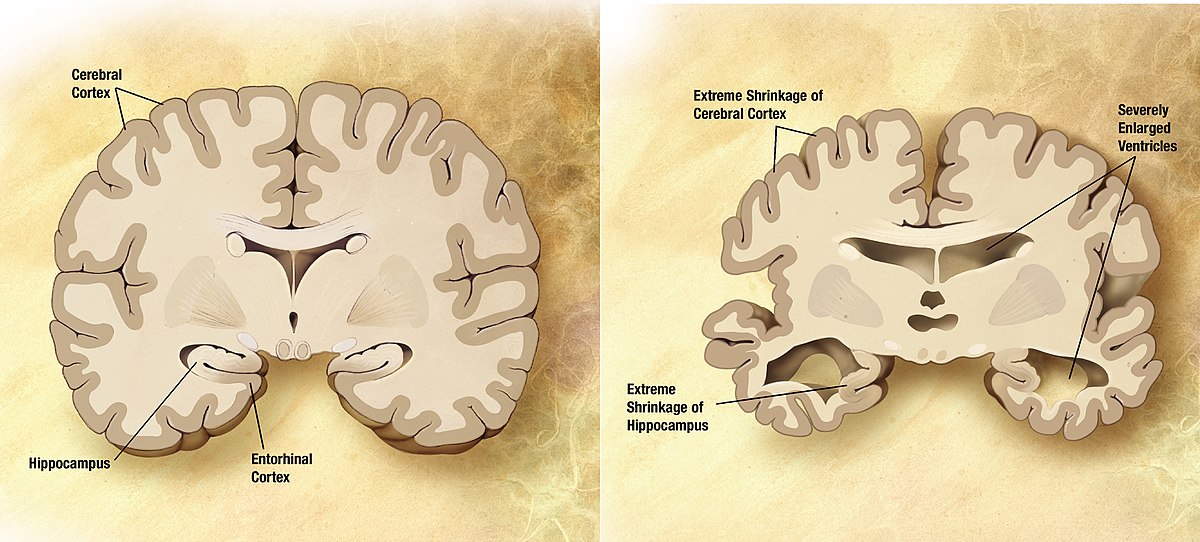
🔬 Pathology
- ⬇️ Acetylcholine in brain/CSF.
- Neurofibrillary tangles: Tau protein inside neurons.
- Senile plaques: β-amyloid deposits in hippocampus, basal forebrain, cortex.
🧬 Genetics
- Rare autosomal dominant: Presenilin 1, Presenilin 2, APP genes.
- ApoE e4 homozygotes at much higher risk.
⚠️ Increased Risks
- Age, family history, traumatic brain injury.
- Diabetes, hypertension, cardiovascular disease.
- Down syndrome.
👩⚕️ Clinical Features
- 📉 Progressive memory loss (esp. episodic memory).
- 🧭 Disorientation, visuospatial difficulty.
- 🖐️ Dyspraxia, agnosia, impaired executive planning.
- 😟 Behavioural: anxiety, irritability, depression, aggression, loss of insight.
🔎 Investigations
- 🧪 Bloods: FBC, U&E, LFTs, TFTs, B12, folate (exclude reversible causes).
- 🖥️ Imaging: CT/MRI → hippocampal atrophy (MRI best for progression).
- EEG: mild nonspecific slowing.
- Histology (post-mortem): tau tangles & β-amyloid plaques.
🧾 Differential Diagnoses
- Dementia with Lewy bodies.
- Vascular dementia.
- Depression (pseudo-dementia).
🎯 Management Goals
- Maximise independence & quality of life.
- Support cognition, mood, behaviour.
- Provide safe environment & social support.
💊 Management
- Specialist assessment in memory clinic.
- Cognitive enhancers:
- Donepezil 5–10 mg daily
- Galantamine 8–24 mg daily
- Rivastigmine 1.5–6 mg BD or transdermal patch
- Memantine (NMDA antagonist)
- Depression: SSRIs.
- Agitation: low-dose antipsychotics (quetiapine, risperidone, olanzapine) — only if severe, non-pharmacological methods first.
- Social services, MDT support (OT, PT, social work, carers, support groups).
🌅 End-of-Life Care
- Focus shifts to palliation, advanced care planning.
- Mortality ~10% per year in advanced disease.
💡 Exam Pearl: Think Alzheimer’s when you see: older patient + progressive memory loss + hippocampal atrophy + no stepwise decline (unlike vascular dementia).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
