| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Anterior / Medial Medullary Infarct (Dejerine Syndrome)
Related Subjects: |Anaromy and Physiology of the Brain |Cryptogenic stroke |Anterior / Medial Medullary Infarct (Dejerine Syndrome)
An anterior (medial) medullary infarct is a brainstem stroke of the medial medulla, usually due to occlusion of the anterior spinal artery or paramedian branches of the vertebral artery. It classically produces a triad of contralateral hemiparesis, contralateral loss of vibration and joint position sense, and ipsilateral hypoglossal palsy. Recognising this pattern helps distinguish it from the more common lateral medullary (Wallenberg) syndrome.
🧬 Vascular Anatomy & Pathophysiology
- The medial medulla is supplied by the anterior spinal artery and small paramedian branches of the vertebral arteries.
- Occlusion causes infarction of:
- Corticospinal tract → contralateral limb weakness.
- Medial lemniscus → contralateral loss of vibration and proprioception.
- Hypoglossal nucleus or exiting XII nerve fibres → ipsilateral tongue weakness.
- Atherosclerosis of the vertebral artery, cardioembolism, or vertebral dissection may underlie the event, especially in younger patients.
📌 Clinical Features (Classic Triad)
- Contralateral hemiparesis (arm and leg) – often pyramidal distribution; face may be relatively spared.
- Contralateral loss of vibration and joint position sense – due to medial lemniscus involvement.
- Ipsilateral hypoglossal palsy – tongue deviates towards the lesion on protrusion, with dysarthria and swallowing difficulty.
Additional/variant features:
- Ataxia from involvement of descending cerebellar pathways.
- Respiratory or cardiovascular instability in extensive lesions.
- Usually no Horner’s syndrome or spinothalamic sensory loss – those point more to lateral medullary infarction.
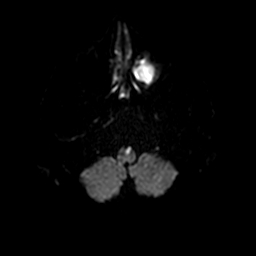
🩻 Imaging
- MRI with DWI is the modality of choice, often showing a “V-shaped” or paramedian lesion in the medial medulla on axial images.
- CTA/MRA should assess vertebral arteries and the origin of the anterior spinal artery for stenosis, occlusion, or dissection.
- CT head is frequently normal early or may show only subtle changes; MRI is often needed for confirmation.
💊 Management
- Acute management follows usual hyperacute stroke protocols – assess for IV thrombolysis and/or thrombectomy according to timing and imaging.
- Secondary prevention as per ischaemic stroke: antiplatelet or anticoagulation (if cardioembolic), statin, BP and risk-factor control, smoking cessation.
- Rehabilitation focuses on bulbar function (swallow, speech), limb weakness, and gait/balance training.
- Monitor for respiratory compromise and aspiration risk; early SALT and nutrition input are often needed.
🧑⚕️ Teaching Pearls
- Think “medial medulla = XII + pyramids + medial lemniscus” → tongue, power, and dorsal-column sensation.
- Crossed signs (ipsilateral cranial nerve, contralateral body) are a big clue to a brainstem lesion.
- Differential includes lateral medullary syndrome, high cervical cord lesions, and internal capsule strokes – the tongue sign helps localise.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
