| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
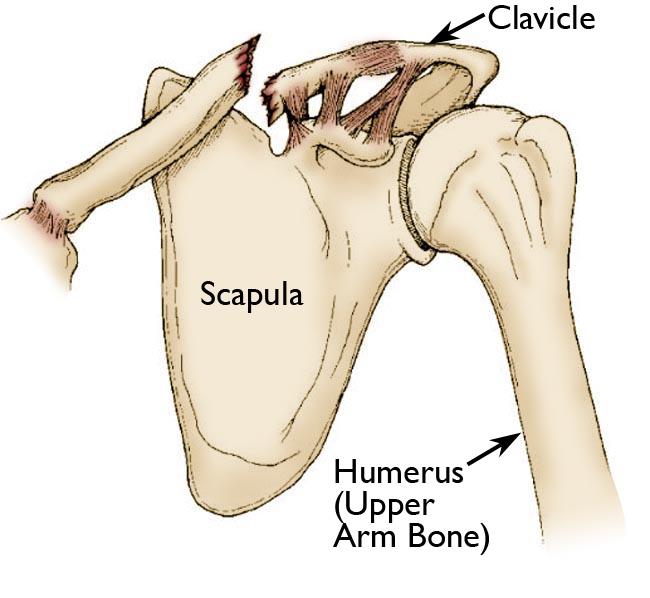
Fractured Clavicle
Clavicle Fractures 🦴 are very common — especially in children and young adults after sports or falls, and in the elderly with osteoporosis. 👉 Most heal well with conservative management. There is no proven long-term functional benefit to surgical fixation in most cases. 🚨 Surgery is reserved for specific indications (open fracture, neurovascular compromise, severe displacement).
📖 About
- Most frequently fractured bone in childhood 👶.
- High-energy sports injuries, FOOSH, or low-impact falls in elderly.
- Up to 80% involve the middle third of the clavicle.
⚙️ Aetiology
- Fall on an outstretched hand (FOOSH) ✋.
- Direct blow to clavicle (contact sports, road traffic accidents 🚲).
- Indirect trauma via shoulder girdle.
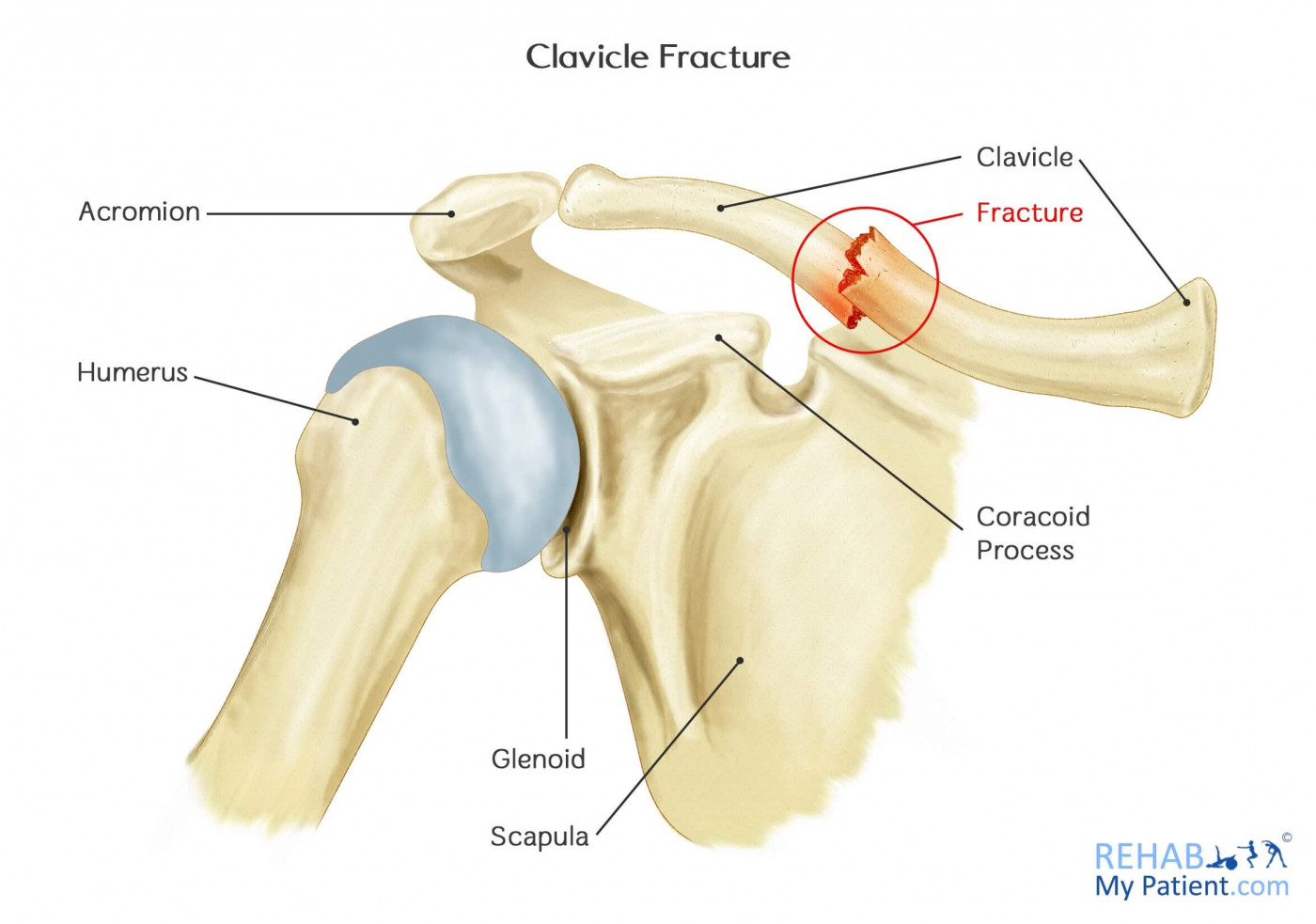
📊 Allman Classification
- Type I (≈80%): Middle third — most common; usually stable.
- Type II (≈15%): Lateral third — often unstable; higher risk of nonunion.
- Type III (≈5%): Medial third — rare, often from major trauma; may involve great vessels or chest injuries.
🔎 Alternative (Neer)
- Further subcategorises lateral third fractures by coracoclavicular ligament involvement → predicts stability and nonunion risk.
🩺 Clinical Features
- Sharp pain over clavicle/shoulder.
- Swelling or deformity over clavicle or anterior chest wall.
- Crepitus/step deformity on palpation.
- Reduced shoulder movement due to pain.
- Systemic response: dizziness, nausea, blurred vision (pain-related).
- Always check for:
- Skin tenting / open wound
- Neurovascular compromise (brachial plexus, subclavian vessels)
- Pneumothorax / haemothorax if medial fracture
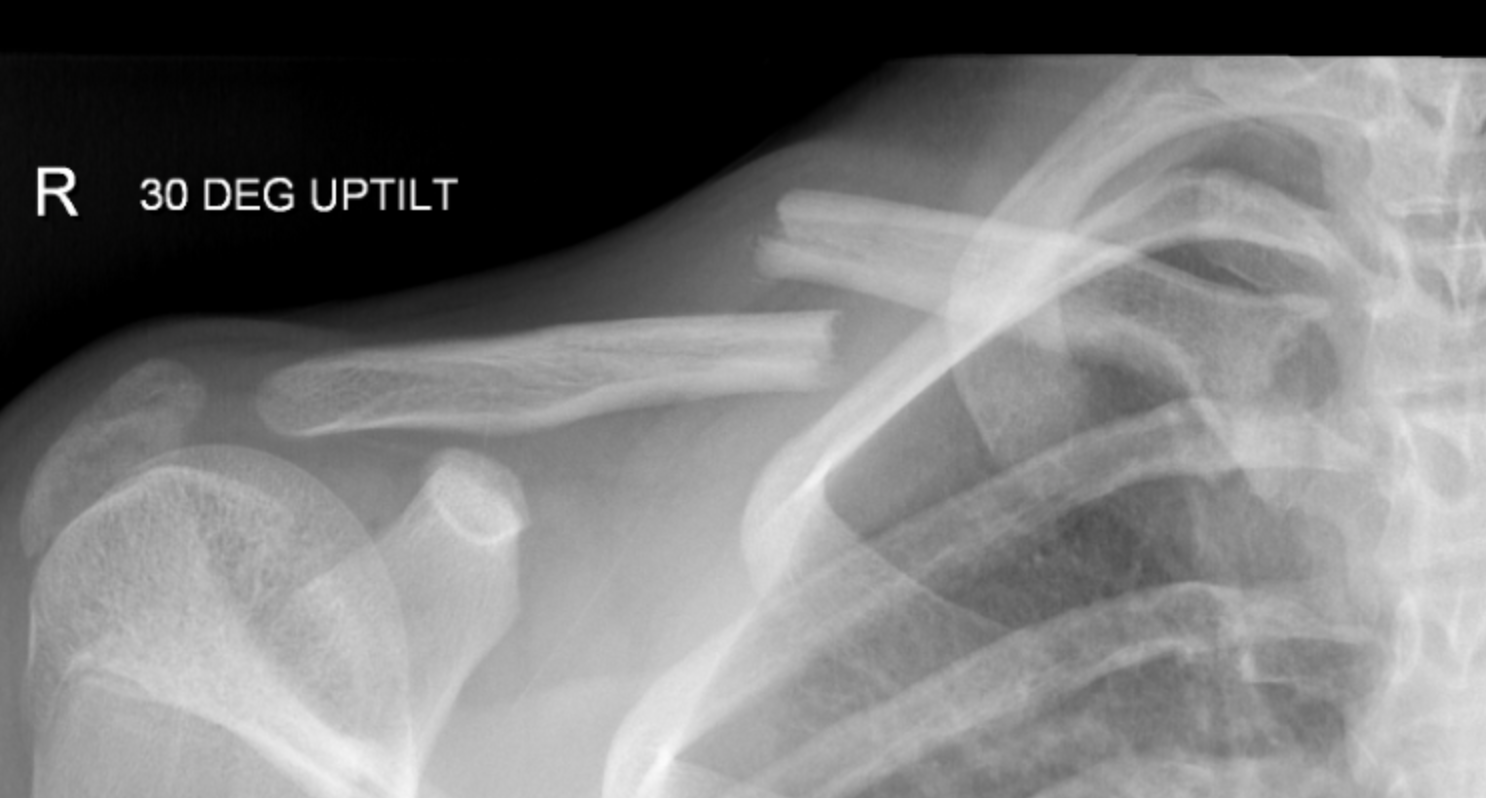
🧪 Investigations
- X-ray: AP clavicle ± 15° cephalic tilt view (best for fracture displacement).
- CT chest: Medial fractures with posterior displacement → exclude mediastinal injury.
- MRI/CT: Rarely, for complex or nonunion cases.
- Ultrasound: Radiation-free and useful in children.
⚠️ Complications
- Nonunion (esp. lateral fractures; risk up to 15%).
- Malunion — bony bump/cosmetic, usually asymptomatic.
- Neurovascular injury — brachial plexus, subclavian artery/vein (rare).
- Pneumothorax / Haemothorax — medial/posterior displacement.
- Infection — only if open or post-surgery.
💊 Management
- Initial: Analgesia, wound care, tetanus prophylaxis if open wound. Document neurovascular status.
- Conservative (majority):
- Broad-arm sling 2–3 weeks until pain allows mobilisation.
- Figure-of-eight brace no longer preferred (no proven benefit).
- Early physiotherapy for ROM once pain settles.
- Children: callus prominence common, remodels with time.
- Surgical Indications (≈5–10%):
- Open fracture or skin tenting (threatened skin) 🚨
- Neurovascular compromise
- Severely displaced/comminuted fracture with >2 cm shortening
- Unstable lateral third fractures (coracoclavicular ligament disruption)
- Symptomatic nonunion
📌 OSCE / Exam Pearls
- Always palpate along entire clavicle — ensure no second injury (esp. sternoclavicular joint).
- Lateral third fractures have highest nonunion risk → consider surgery earlier.
- In children, remodelling is excellent; reassure about cosmetic bumps.
- Check for neurovascular compromise (subclavian vessels, brachial plexus) in displaced medial injuries.
📚 References
- Rockwood & Green’s Fractures in Adults, 9th ed.
- British Orthopaedic Association (BOA) guidance on clavicle fractures.
- Robinson CM. Fractures of the clavicle in the adult. J Bone Joint Surg Br. 1998;80(3):476-484.
- NICE Clinical Knowledge Summaries (CKS): Clavicle fracture. 2023.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
