| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Acute Pancreatitis
Related Subjects: | Acute Cholecystitis | Acute Appendicitis | Chronic Peritonitis | Abdominal Aortic Aneurysm | Ectopic Pregnancy | Acute Cholangitis | Acute Abdominal Pain/Peritonitis | Assessing Abdominal Pain | Penetrating Abdominal Trauma | Acute Pancreatitis | Acute Diverticulitis
🧪 Lipase vs Amylase: Lipase is more useful than amylase as it is equally sensitive but more specific, and it remains elevated for longer. - ⏳ Lipase half-life: 8–14 days (vs 3–5 days for amylase). - 🚫 Lipase levels do not correlate with severity. - ✅ Particularly useful in delayed presentation of acute pancreatitis.
| ⚡ Initial Management of Acute Pancreatitis |
|---|
|
ℹ️ About
- 📉 Poor correlation between amylase level and severity.
- 🔥 Acute inflammation releases amylase, lipase, trypsin → autodigestion.
- ⚠️ Significant morbidity & mortality; may trigger SIRS and multi-organ failure.
- 📈 Incidence rising due to ↑ alcohol use & improved detection.
🎯 Causes
- 🪨 Gallstones (most common UK)
- 🍷 Alcohol
- 🧬 Pancreatic cancer, post-ERCP
- 📈 Hypertriglyceridaemia, hyperparathyroidism
- 💊 Drugs: steroids, thiazides, azathioprine, sulphonamides, fibrates, statins, ART drugs, valproate, cisplatin, erythromycin
- 🦟 Infections: HIV, CMV, EBV
- 🪲 Trauma, snake bite (rare)
🩺 Diagnosis (need 2 of 3)
- Severe epigastric pain radiating to back
- ↑↑ Amylase or Lipase (>3 × ULN)
- Imaging (USS/CT/MRI) consistent with pancreatitis
🧬 Aetiology / Pathophysiology
- Premature activation of pancreatic enzymes (trypsin, lipase, amylase) → autodigestion → fat necrosis, haemorrhage, inflammation → SIRS.
🩹 Clinical Features
- 🔥 Severe epigastric pain radiating to back, relieved by sitting forward
- 🤢 Nausea, vomiting
- 📉 Shock: tachycardia, hypotension, fever
- ⚠️ Grey Turner’s sign (flank bruising), Cullen’s sign (periumbilical bruising)
📊 Prognosis – Ranson’s Criteria
- At admission: Age >55, WCC >16,000, Glucose >11, LDH >350, AST >600
- At 48h: Hct fall >10%, Ca²⁺ <2, PaO₂ <8 kPa, BE < -4, Urea rise >1.8, Fluid needs >6L
📉 Mortality by Criteria
- 0–2: <5%
- 3–4: 20%
- 5–6: 40%
- 7–8: ≈100%
🔬 Investigations
- FBC, U&E, Ca²⁺, LFTs, LDH, Albumin, CRP, ABG
- Lipids (↑ triglycerides)
- Amylase (↑ but non-specific); Lipase (↑, more specific)
- USS: within 24 hrs for gallstones
- CT: within 7–10 days for severe cases, contrast-enhanced
- ERCP: if gallstone pancreatitis + cholangitis or obstruction
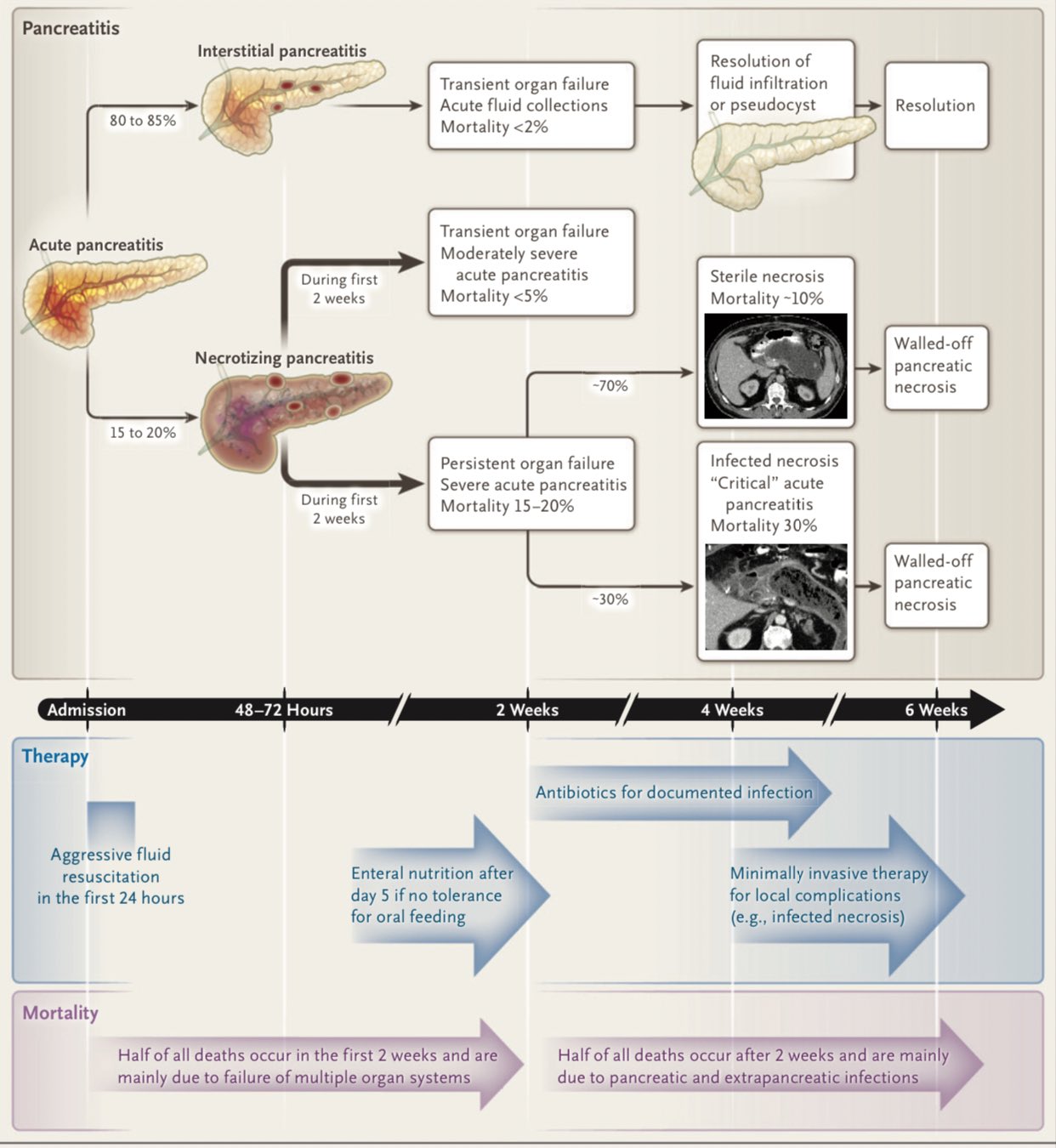
⚠️ Complications
- 🫀 Local: necrosis, pseudocyst, abscess
- 🫁 Systemic: ARDS, sepsis, renal failure, hypocalcaemia
- ➡️ Chronic pancreatitis if recurrent
💊 Ongoing Management
- 🔄 ABC resuscitation, IV fluids, catheter
- 💊 Analgesia (opioids), antiemetics
- 🥤 NBM initially; enteral feeding if prolonged
- 🧪 Antibiotics only if proven infection
- 🩻 ERCP + sphincterotomy within 72 hrs if gallstone pancreatitis
- 🔪 Necrosectomy for infected necrosis/abscess
- 🏥 HDU/ICU if organ dysfunction
🩺 Case 1 — Gallstone Pancreatitis
A 52-year-old woman presents with sudden severe epigastric pain radiating to the back, nausea, and vomiting. She has a history of gallstones. Labs: amylase 900 U/L, lipase elevated, ALT high. USS shows gallstones without duct dilatation. Management: 🏥 Admit, IV fluids, analgesia, antiemetics, and monitor for systemic complications. ERCP if cholangitis or obstructive jaundice. Definitive management = laparoscopic cholecystectomy. Avoid: ❌ Routine prophylactic antibiotics; avoid oral intake until pain and vomiting controlled.
🩺 Case 2 — Alcohol-Related Pancreatitis with Pseudocyst
A 45-year-old man with chronic alcohol use presents with acute epigastric pain and vomiting. He is managed supportively but continues to have persistent abdominal fullness 4 weeks later. CT abdomen shows a 6 cm pancreatic pseudocyst. Management: 💊 Supportive care during acute phase (fluids, analgesia, electrolyte balance). Large or symptomatic pseudocyst → endoscopic or surgical drainage. Refer to alcohol services. Avoid: ❌ Draining a pseudocyst too early (<4 weeks) as the wall may not be mature; avoid NSAIDs in renal impairment from pancreatitis.
🩺 Case 3 — Severe Pancreatitis with Necrosis
A 63-year-old man presents with severe pancreatitis due to hypertriglyceridaemia. He develops hypotension, tachycardia, hypoxia, and rising CRP. CT scan shows necrotising pancreatitis with areas of non-enhancing pancreas. Management: 🚑 Admit to HDU/ICU, aggressive IV fluid resuscitation, oxygen support, nutritional support (NG feeding). If infected necrosis, consider broad-spectrum antibiotics and surgical or radiological debridement. Avoid: ❌ Prophylactic antibiotics for sterile necrosis; avoid morphine derivatives that may cause sphincter of Oddi spasm (pethidine historically preferred, though in practice morphine still used with care).
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
