Makindo Medical Notes"One small step for man, one large step for Makindo" |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER: The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis, or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd. |
Cerebral Venous Thrombosis (CVT)
Related Subjects: Thrombophilia testing |Antiphospholipid syndrome |Protein C Deficiency |Protein S Deficiency |Prothrombin 20210A mutation |Factor V Leiden Deficiency |Antithrombin III deficiency (AT3) |Cerebral Venous Sinus thrombosis |Budd-Chiari syndrome
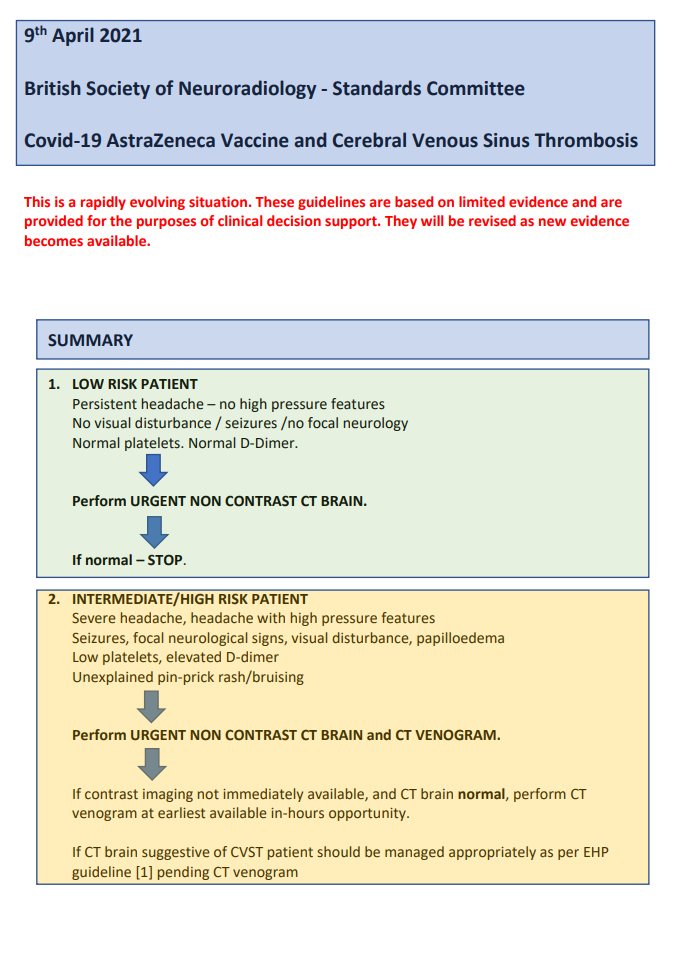
🧠 Cerebral Venous Thrombosis (CVT) is an under-recognised cause of stroke, especially in young adults, postpartum women, and patients with prothrombotic conditions. ⚠️ Postpartum period is a major risk factor, and CVST has also been reported rarely in association with COVID-19 vaccination + thrombocytopenia. Clues: persistent headache, papilloedema, seizures, or infarcts not in arterial territories.
📖 About
- Likely underdiagnosed; many cases are missed or treated late.
- Headache + papilloedema + normal CT should raise suspicion.
- Think of CVST in pregnant/postpartum women or patients with prothrombotic risk factors.
⚙️ Aetiology (Causes)
- 💊 OCP use, pregnancy, postpartum period.
- 💉 Procoagulant states: Factor V Leiden, protein C/S deficiency, antithrombin deficiency, prothrombin mutation, hyperhomocysteinaemia.
- 🩸 Haematological: polycythaemia, thrombocythaemia, leukaemia, sickle cell disease.
- 🦠 Infections: mastoiditis, otitis media, sinusitis, bacterial meningitis.
- 🧬 Systemic conditions: Behçet’s, SLE, ulcerative colitis, Crohn’s, APS, Graves’ disease.
- ⚡ Drugs: Ecstasy (MDMA), chemotherapy.
- 🦴 Trauma/neurosurgery near venous sinuses.
- 🦠 Malignancy: adenocarcinomas, haematological cancers.
- 💉 Post-COVID-19 vaccine (rare): CVST with thrombocytopenia/VITT.
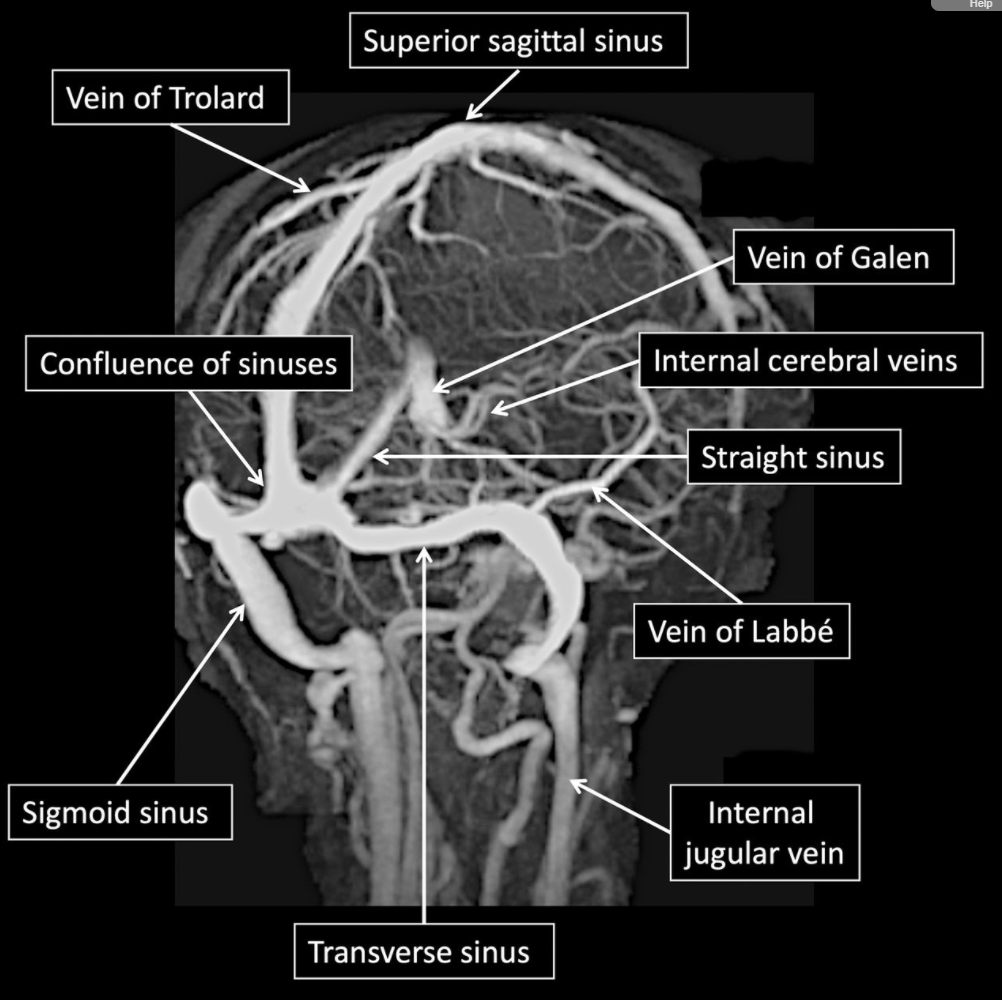
🧭 Venous Anatomy
CVST can affect any venous sinus or cortical vein, leading to raised ICP and venous infarction.
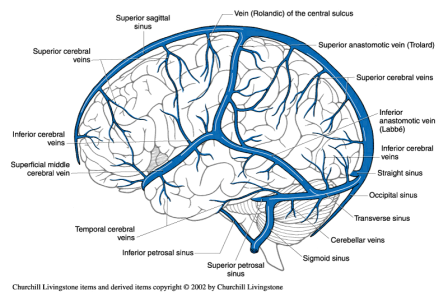
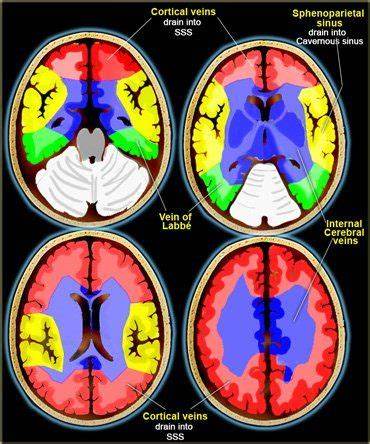
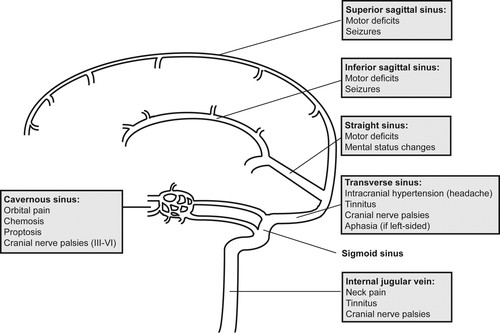
🩸 Common Sites & Clinical Patterns
- Superior sagittal sinus: raised ICP, headache, papilloedema.
- Lateral/straight sinus, vein of Galen: bilateral thalamic infarcts → akinetic mutism.
- Small cortical veins: focal cortical signs, seizures.
- Cavernous sinus: cranial neuropathies, proptosis, cavernous sinus syndrome.
🔬 Pathophysiology
- Obstruction of venous outflow → venous congestion, cytotoxic + vasogenic oedema.
- Haemorrhagic venous infarction due to capillary rupture.
- ↓ CSF absorption via arachnoid granulations → raised ICP.
- Subarachnoid haemorrhage may occasionally occur.
🩺 Clinical Presentation
- 💢 Headache in ~90% (often progressive, worse lying down).
- 🌡️ Raised ICP: papilloedema, nausea, vomiting, sixth nerve palsy.
- ⚡ Seizures: focal or generalised (much more common than in arterial stroke).
- 🧑⚕️ Focal neurology: hemiparesis, aphasia, cortical signs.
- 🤒 Cavernous sinus thrombosis: ophthalmoplegia, cranial nerve palsies, facial pain.
- 🌀 Atypical: psychosis, encephalopathy, TIA-like symptoms, migraine-like headache.
🧾 Differential Diagnosis
- Idiopathic intracranial hypertension (IIH): important mimic, especially in young obese women. ➡️ If male or non-obese, always exclude CVST.
🔍 Investigations
- 🩸 FBC: Look for thrombocytopenia (consider VITT, HIT, leukaemia).
- 🧪 D-dimer: Usually raised but not fully sensitive.
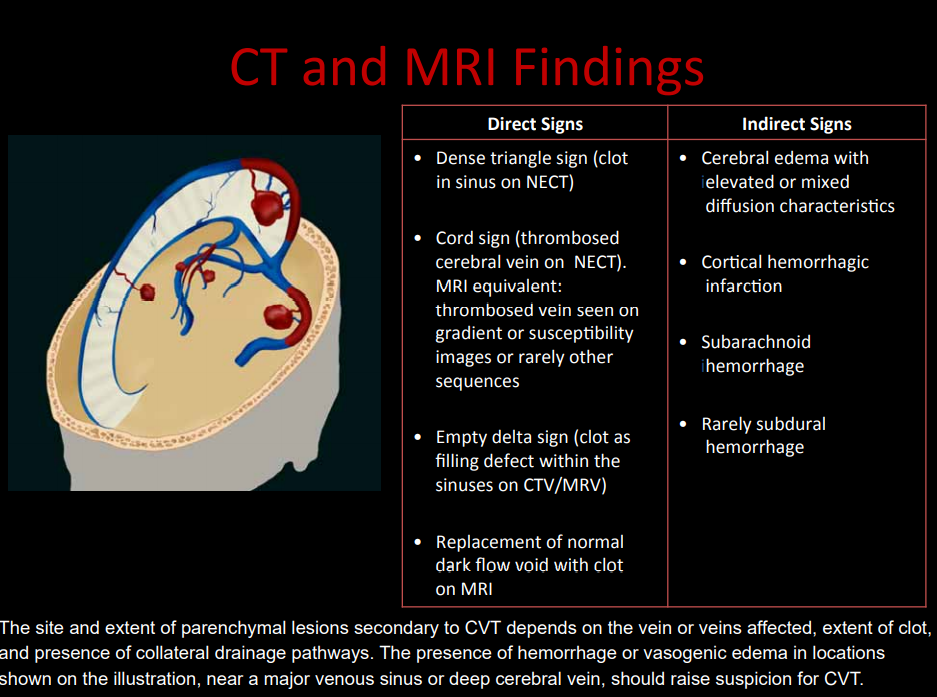
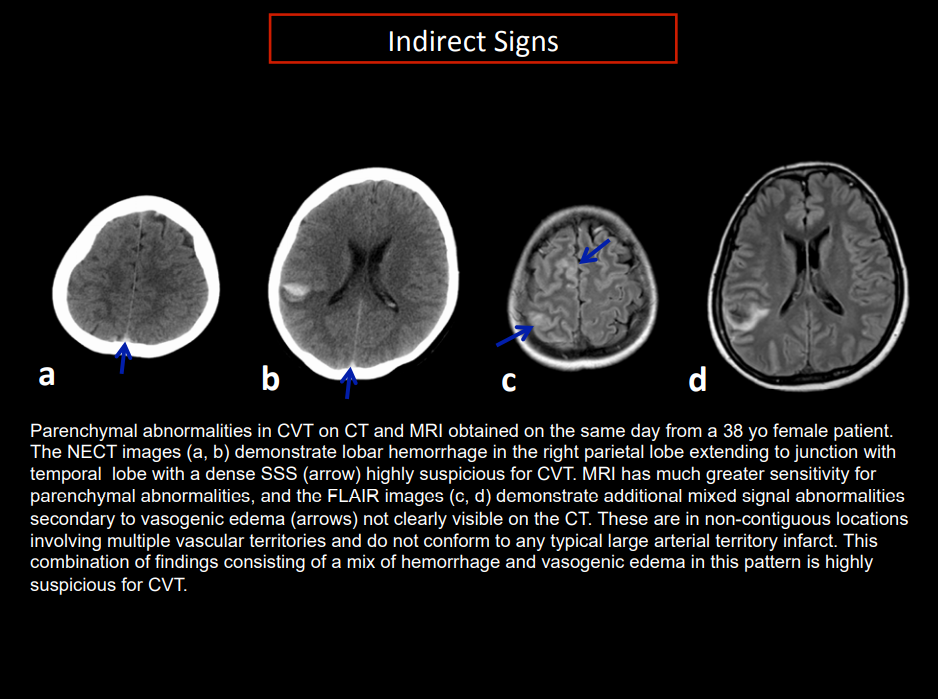
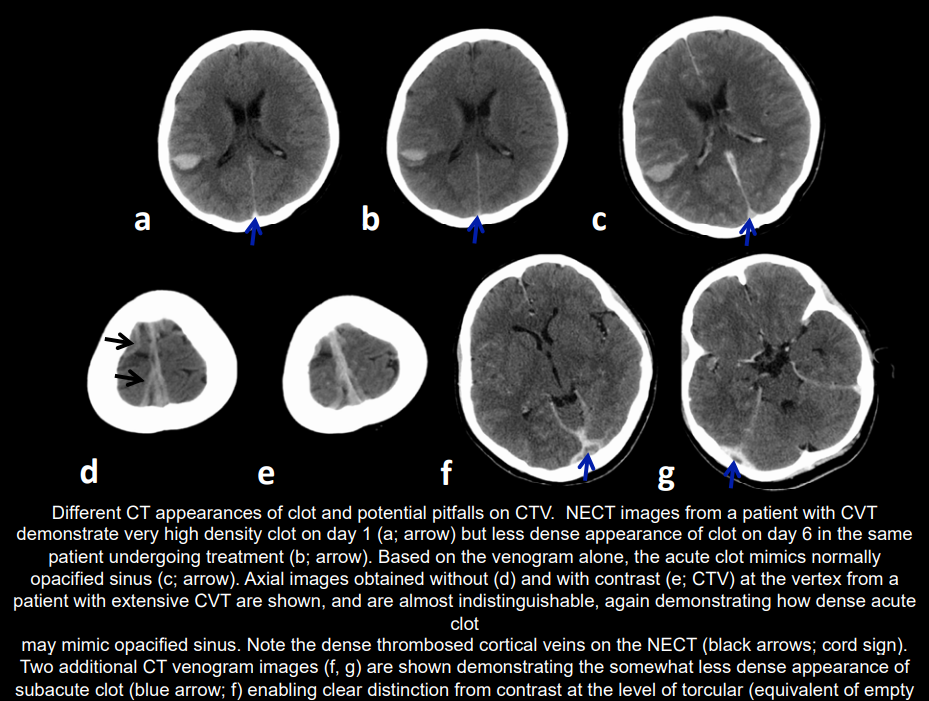
- 🖼️ CT (plain): May be normal; may show haemorrhagic infarcts not in arterial territories. "Cord sign" (fresh clot), SAH possible.
- 🩻 CT venography: "Empty delta sign" (contrast around clot in sagittal sinus).
- 🧲 MRI/MRV: Best modality. Detects venous clot, oedema, infarction, haemorrhage.
- 💉 CSF: ↑ opening pressure, ↑ protein; WCC mildly raised.
- 🧬 Thrombophilia screen: Factor V Leiden, prothrombin G20210, protein C/S deficiency, antithrombin deficiency, homocystinuria.
📉 Prognosis Factors
- Deep venous involvement → poor prognosis (bilateral thalamic infarcts).
- Male sex associated with worse outcomes.
- Right lateral sinus thrombosis carries higher risk.
🧬 Inherited Procoagulant Conditions (approx. prevalence)
- Factor V Leiden: 3–7%.
- Prothrombin G20210 mutation: 1–2%.
- Protein C deficiency: 0.3%.
- Protein S deficiency: 0.1%.
- Antithrombin deficiency: 0.02%.
⚖️ Management
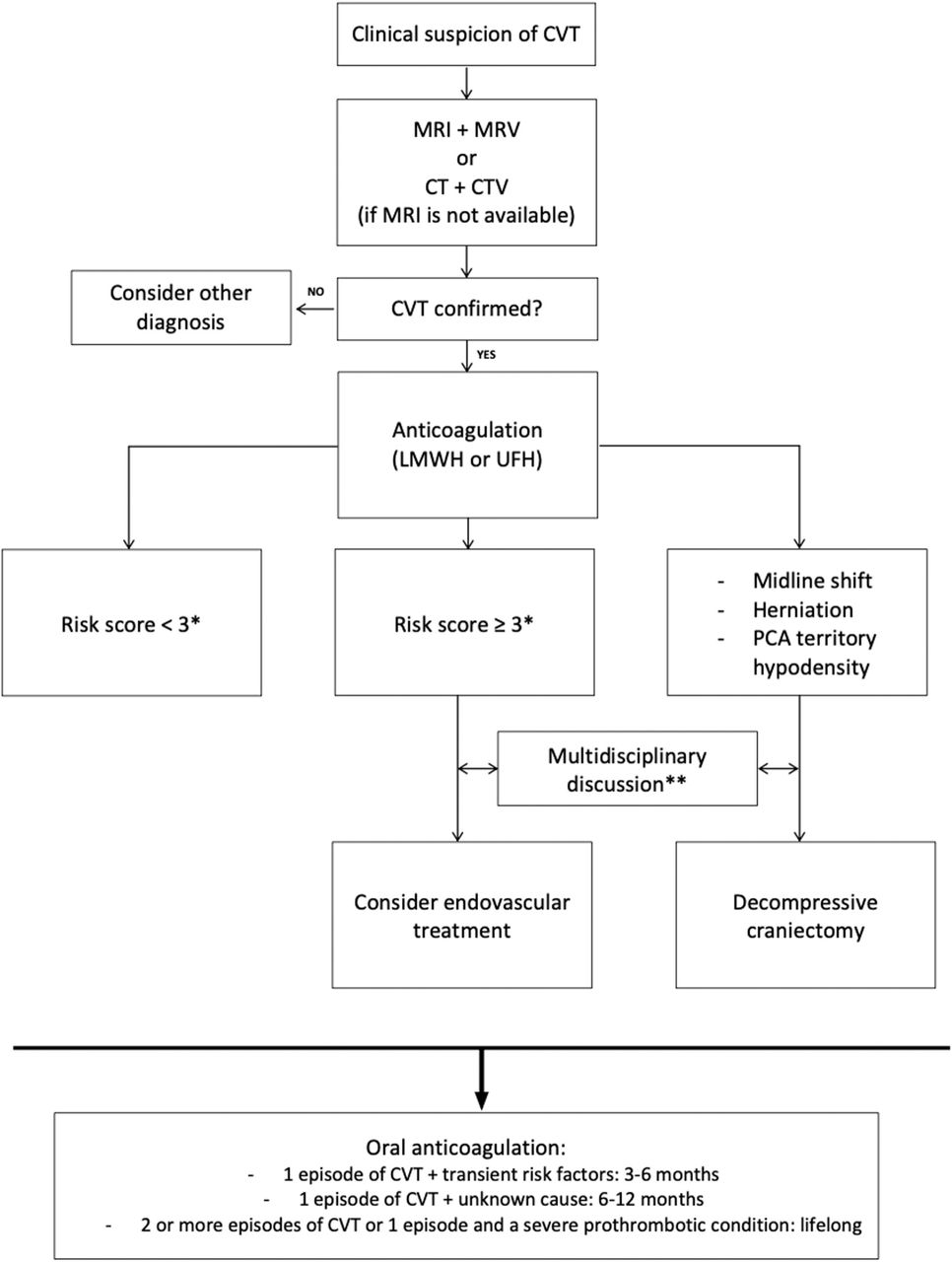
- 💉 Anticoagulation is the cornerstone: LMWH preferred (BID dosing). UFH if renal failure or rapid reversal required.
- 🩸 Even with haemorrhagic venous infarcts, anticoagulation is not contraindicated.
- 🔄 Oral anticoagulation (warfarin, INR 2–3) for 3–12 months; longer if recurrent or idiopathic.
- ⚡ Endovascular thrombolysis/thrombectomy: for severe/refractory cases in expert centres.
- 📉 COVID-19 related (VITT): avoid heparin, use IVIG + non-heparin anticoagulants (e.g., argatroban, fondaparinux) per guidelines.
- 🧑⚕️ Supportive: ICP management (acetazolamide, CSF drainage if needed), seizure prophylaxis if recurrent.
📚 References
- Cerebral venous thrombosis: a practical guide. Pract Neurol 2020.
- Imaging Approach to CVST – CAR.
- Piazza G. Circulation 2012;125:1704–1709.
- ACC: CVST with Vaccine-Induced Thrombocytopenia.
💡 Exam Pearls:
– CVST = young woman + headache + seizures + haemorrhagic infarct not in arterial territory.
– Always request CT/MR venography if suspicion is high.
– Anticoagulation is safe, even with haemorrhage.
Categories
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology