| Download the amazing global Makindo app: Android | Apple | |
|---|---|
| MEDICAL DISCLAIMER: Educational use only. Not for diagnosis or management. See below for full disclaimer. |
Ischaemic Strokes in the Pons
Related Subjects: |Anatomy the Medulla Oblongata |Anatomy of the Midbrain |Anatomy of the Pons
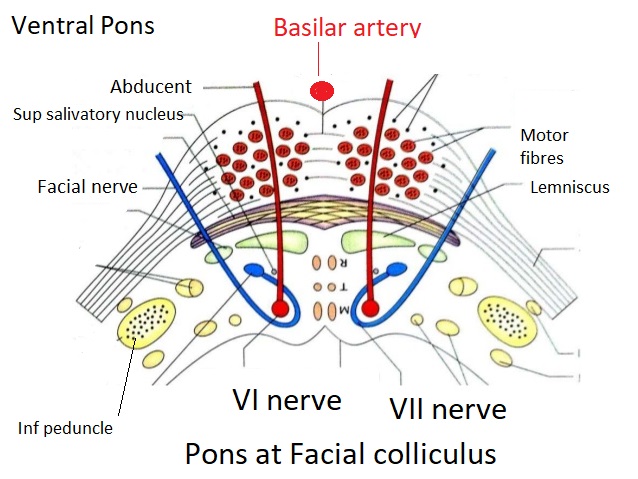
🧠 Note: Anatomical diagrams of the pons are often displayed inverted compared to radiological (CT/MRI) orientation — except as shown below. This distinction is important when correlating anatomy with clinical findings or interpreting imaging.
🌉 Introduction
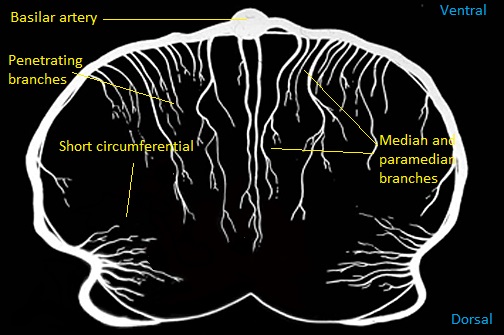
- 🩸 Pontine strokes are most often lacunar infarcts due to occlusion of small penetrating arteries from the basilar trunk.
- 📈 Common risk factors include age, hypertension, diabetes, and atherosclerosis.
- ⚠️ Bilateral lesions are uncommon but can occur with basilar artery occlusion — potentially devastating with “locked-in” presentation.
🧬 Aetiology
- 🎯 Usually small-vessel occlusion of penetrating branches of the basilar artery → unilateral pontine infarcts.
- 🫀 Basilar occlusion at the origins of perforators → possible bilateral pontine infarction.
- 🔄 Shared risk factors with other small-vessel strokes: hypertension, diabetes, ageing, and lipohyalinosis.
- 🚫 Large-vessel infarcts (basilar atherothrombosis, embolism) → wider territory infarction ± coma.
- 💧 Oedema near 4th ventricle may obstruct CSF flow → acute hydrocephalus requiring ventricular drainage.
🧩 Clinical Features
- ⚡ Contralateral hemiparesis or hemisensory loss — corticospinal and medial lemniscus involvement.
- 🚫 No cortical signs (e.g., aphasia, neglect, hemianopia) — helps differentiate from cortical stroke.
- 🙂 Ipsilateral facial palsy (LMN type) — facial nucleus or fascicle lesion.
- 👀 Diplopia or lateral gaze palsy — due to abducens (VI) nerve involvement.
- 🔒 Locked-in syndrome: Quadriplegia + anarthria but preserved consciousness and vertical eye movement.
- 🌀 Vertigo, nystagmus, ataxia — if cerebellar peduncles affected.
- 🔥 Pyrexia & autonomic instability — involvement of reticular or hypothalamic pathways.
- 🗣️ Dysarthria–clumsy hand syndrome or pure motor stroke presentations (lacunar syndromes).
- 🔁 Fluctuating symptoms — “pontine warning syndrome”, similar to capsular warning episodes.
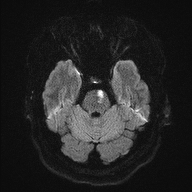
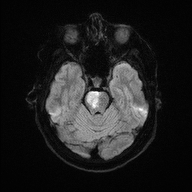
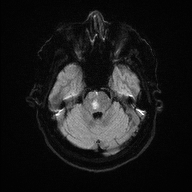
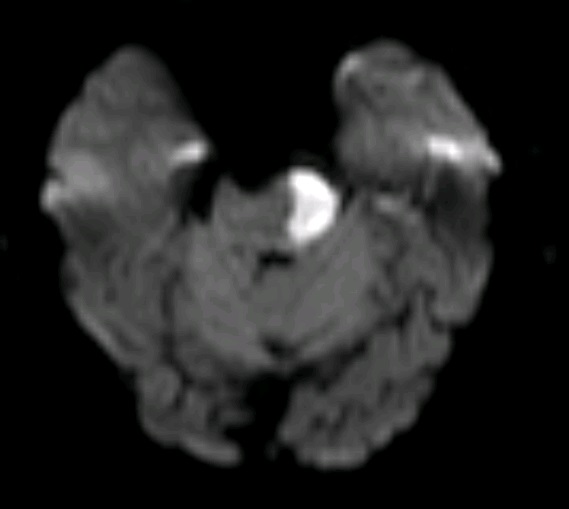
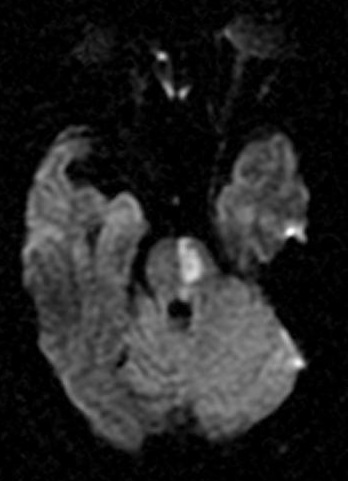
🖼️ Anatomical & Imaging Examples
📍 Pontine infarcts typically respect the midline and may extend posteriorly toward the cerebellum.

🧪 Investigations
- 🩸 Routine bloods: FBC, U&E, LFTs, glucose, lipid profile.
- 🧠 CT ± CTA: To confirm acute stroke, rule out haemorrhage, and assess basilar patency.
- 🧲 MRI brain: More sensitive for small infarcts — DWI highlights acute ischaemia early.
- 🔍 MRA / CTA: Evaluate for vertebrobasilar stenosis or occlusion.
🩺 Management
- 💉 Reperfusion therapy: IV thrombolysis (within window) or thrombectomy for basilar occlusion — improves survival in selected patients.
- 🏥 Stroke Unit care: Multidisciplinary monitoring, oxygenation, and early rehab initiation.
- 💊 Antiplatelet: Aspirin 300 mg ± Clopidogrel after imaging confirms ischaemia.
- ⚖️ Risk factor control: Optimize BP, glucose, and address AF or dyslipidaemia.
- 🧠 Statins: Start high-intensity statin (e.g., atorvastatin 80 mg) for secondary prevention.
- 🗣️ Rehabilitation: Physiotherapy, occupational therapy, and speech therapy for motor/speech recovery and swallow safety.
💡 Teaching tip: Pontine strokes are often clinically silent or subtle initially but may deteriorate rapidly. Always assess eye movements, facial symmetry, and bulbar function in any suspected brainstem event. Locked-in syndrome is the hallmark of extensive bilateral pontine infarction — preserved awareness but paralysis below the eyes.
Categories
- A Level
- About
- Acute Medicine
- Anaesthetics and Critical Care
- Anatomy
- Anatomy and Physiology
- Biochemistry
- Book
- Cardiology
- Collections
- CompSci
- Crib Sheets
- Crib sheets
- Dental
- Dermatology
- Differentials
- Drugs
- ENT
- Education
- Electrocardiogram
- Embryology
- Emergency Medicine
- Endocrinology
- Ethics
- Foundation Doctors
- GCSE
- Gastroenterology
- General Practice
- Genetics
- Geriatric Medicine
- Guidelines
- Gynaecology
- Haematology
- Hepatology
- Immunology
- Infectious Diseases
- Infographic
- Investigations
- Lists
- Mandatory Training
- Medical Students
- Microbiology
- Nephrology
- Neurology
- Neurosurgery
- Nutrition
- OSCE
- OSCEs
- Obstetrics
- Obstetrics Gynaecology
- Oncology
- Ophthalmology
- Oral Medicine and Dentistry
- Orthopaedics
- Paediatrics
- Palliative
- Pathology
- Pharmacology
- Physiology
- Procedures
- Psychiatry
- Public Health
- Radiology
- Renal
- Respiratory
- Resuscitation
- Revision
- Rheumatology
- Statistics and Research
- Stroke
- Surgery
- Toxicology
- Trauma and Orthopaedics
- USMLE
- Urology
- Vascular Surgery
